J Korean Assoc Oral Maxillofac Surg.
2010 Dec;36(6):497-501.
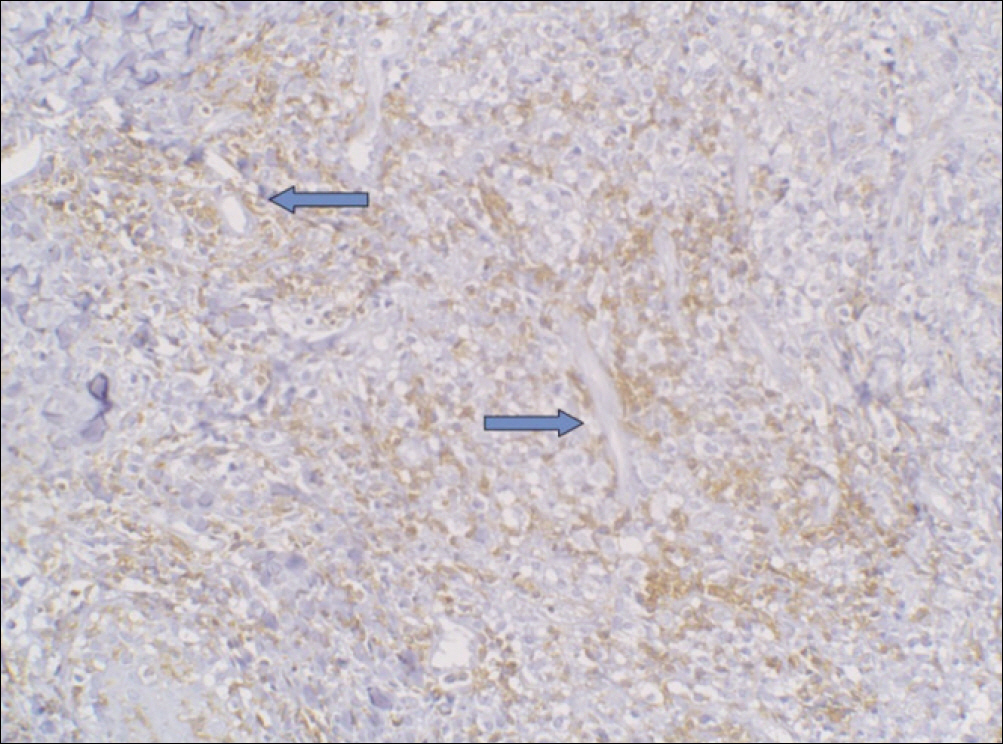
Extranodal NK/T cell Lymphoma, nasal type: clinical, radiological, histological features for early diagnosis
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, College of Dentistry, Yonsei University, Seoul, Korea. kimoms@yuhs.ac
- 2Department of Oral Pathology, College of Dentistry, Yonsei University, Seoul, Korea.
- 3Oral Cancer Research Institute, College of Dentistry, Yonsei University, Seoul, Korea.
Abstract
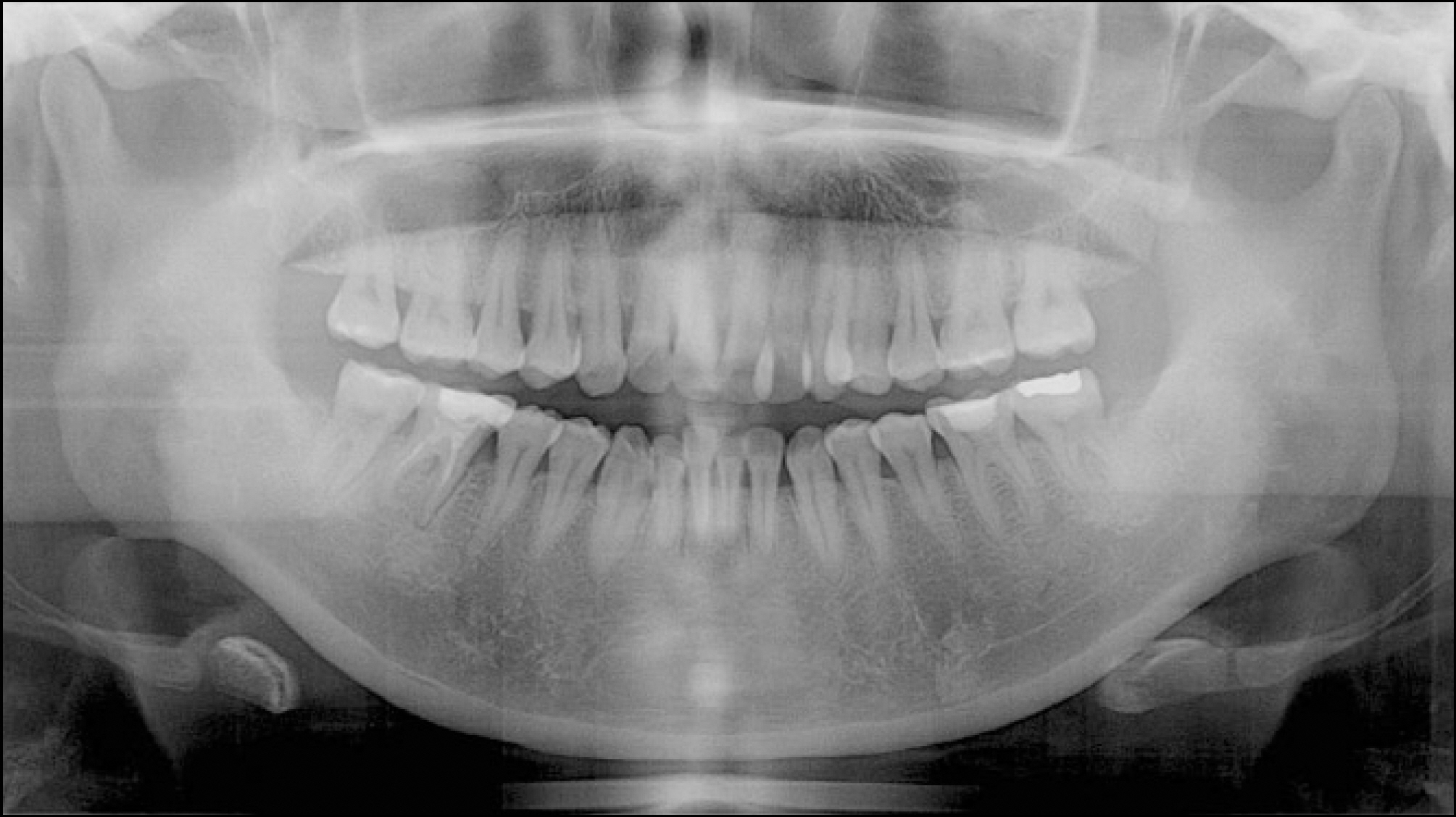
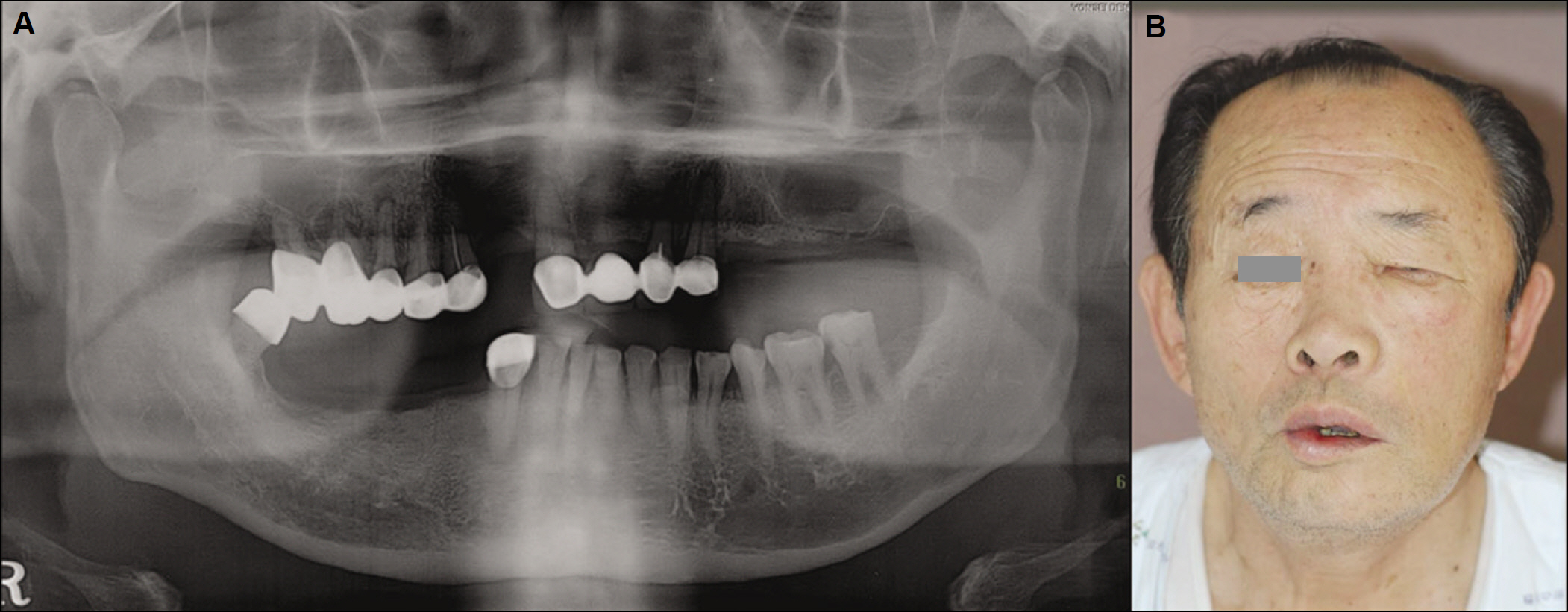
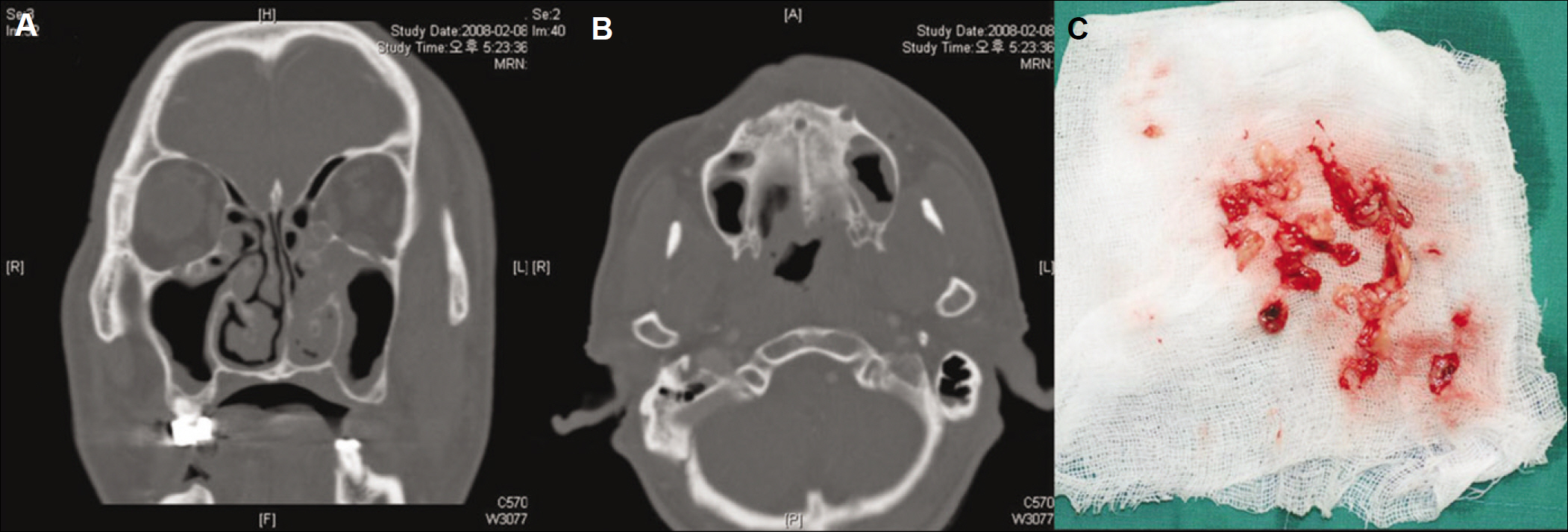
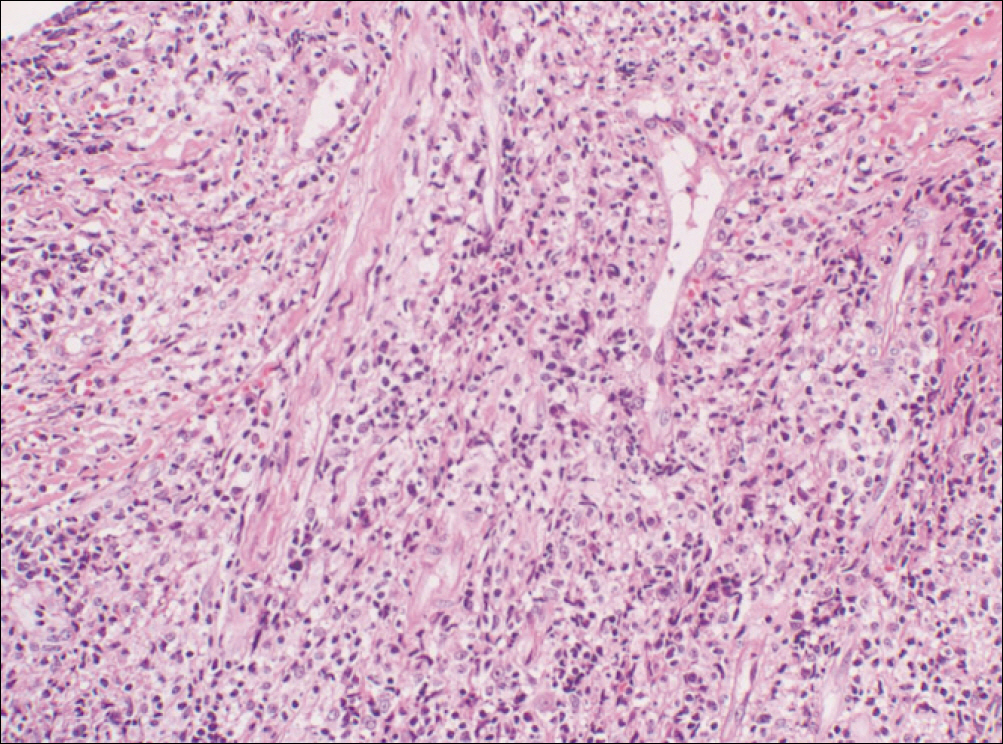
- Primary nasal type natural killer (NK)/T cell (NKTC) lymphoma, a specific form of malignant lymphoma, has a higher geographic incidence in Oriental, Mexican, and South American populations than the Western population. In Koreans, it comprises 9-12% of all cases of non-Hodgkin's lymphoma. This type of lymphoma has also been named as angiocentic lymphoma and lethal midline granuloma because the most common site is the upper airway area and its clinical aggressiveness presents with a necrotic and destructive pattern. NKTC lymphoma can also be detected in different organs (testis, spleen, parotid gland, skin, gastroinstinal tract, central nervous system, lungs, bone marrow, etc.) other than the upper airway including the oral cavity. The lymphoma detected in the oral cavity shows various destructive and inflammatory changes, similar to the signs of inflammation and infection from periodontitis and pulpal disease, making a diagnosis difficult with just the clinical signs. For early detection, clinical, radiological, and pathological examinations are required. This report describes the clinical, radiological and histological characteristics with a case report for the early detection of NKTC lymphoma in the oral cavity.
Keyword
MeSH Terms
Figure
Reference
-
1. Suzuki R, Takeuchi K, Ohshima K, Nakamura S. Extranodal NK/T-cell lymphoma: diagnosis and treatment cues. Hematol Oncol. 2008; 26:66–72.
Article2. Lu P. Staging and classification of lymphoma. Semin Nucl Med. 2005; 35:160–4.
Article3. Kim J, Kim EY, Lee SK, Kim DI, Kim CH, Kim SH, et al. Extranodal nasal-type NK/T-cell lymphoma: computed tomography findings of head and neck involvement. Acta Radiol. 2010; 51:164–9.
Article4. Harabuchi Y, Takahara M, Kishibe K, Moriai S, Nagato T, Ishii H. Nasal natural killer (NK)/T-cell lymphoma: clinical, histological, virological, and genetic features. Int J Clin Oncol. 2009; 14:181–90.
Article5. Ko YH, Cho EY, Kim JE, Lee SS, Huh JR, Chang HK, et al. NK- and NK-like T-cell lymphoma in extranasal sites: a comparative clinicopathological study according to site and EBV status. Histopathology. 2004; 44:480–9.
Article6. Al-Hakeem DA, Fedele S, Carlos R, Porter S. Extranodal NK/T-cell lymphoma, nasal type. Oral Oncol. 2007; 43:4–14.
Article7. Chiang AK, Chan AC, Srivastava G, Ho FC. Nasal T/natural killer (NK)-cell lymphomas are derived from Epstein-Barr virus-infected cytotoxic lymphocytes of both NK-,!,!,!,! and T-cell lineage. Int J Cancer. 1997; 73:332–8.
Article8. Seishima M, Yuge M, Kosugi H, Nagasaka T. Extranodal NK/T-cell lymphoma, nasal type, possibly arising from chronic Epstein-Barr virus infection. Acta Derm Venereol. 2010; 90:102–3.
Article9. Ko YH, Ree HJ, Kim WS, Choi WH, Moon WS, Kim SW. Clinicopathologic and genotypic study of extranodal nasal-type natural killer/T-cell lymphoma and natural killer precursor lymphoma among Koreans. Cancer. 2000; 89:2106–16.
Article10. Peh SC, Quen QW. Nasal and nasal-type natural killer (NK)/T-cell lymphoma: immunophenotype and Epstein-Barr virus (EBV) association. Med J Malaysia. 2003; 58:196–204.11. Chan JK, Sin VC, Wong KF, Ng CS, Tsang WY, Chan CH, et al. Nonnasal lymphoma expressing the natural killer cell marker CD56: a clinicopathologic study of 49 cases of an uncommon aggressive neoplasm. Blood. 1997; 89:4501–13.
Article12. Garcl′a-Cosl′o M, Santo′n A, Me′ndez MC, Rivas C, Martl′n C, Bellas C. Nasopharyngeal/nasal type T/NK lymphomas: analysis of 14 cases and review of the literature. Tumori. 2003; 89:278–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extranodal NK/T Cell Lymphoma, Nasal Type that Occurred in Patients with Atrophic Rhinitis
- A Case of Extranodall NK/T-cell Lymphoma, Nasal type
- A Case of Nasal Extranodal NK/T Cell Lymphoma Misdiagnosed as Reccurent Periorbital Cellulitis or Acute Dacryocystitis
- A Case of Extranodal Natural Killer/T Cell Lymphoma Combined With Actinomycosis
- Delayed Diagnosis Due to Septal Perforation in Patient with Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type