Infect Chemother.
2016 Jun;48(2):81-90. 10.3947/ic.2016.48.2.81.
Prolonged versus Intermittent Infusion of β-Lactams for the Treatment of Nosocomial Pneumonia: A Meta-Analysis
- Affiliations
-
- 1The Veterans Affairs Western New York Healthcare System, Buffalo, NY, USA. solh@buffalo.edu, pea@buffalo.edu
- 2Western New York Respiratory Research Center, Division of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine and Department of Social and Preventive Medicine, State University of New York at Buffalo School of Medicine and Biomedical Scie
- 3School of Public Health and Health Professions, Buffalo, NY, USA.
- KMID: 2327975
- DOI: http://doi.org/10.3947/ic.2016.48.2.81
Abstract
- BACKGROUND
The primary objective of this meta-analysis is aimed at determining whether β-lactams prolonged infusion in patients with nosocomial pneumonia (NP) results in higher cure rate and improved mortality compared to intermittent infusion.
MATERIALS AND METHODS
Relevant studies were identified from searches of MEDLINE, EMBASE, and CENTRAL from inception to September 1st, 2015. All published articles which evaluated the outcome of extended/continuous infusion of antimicrobial therapy versus intermittent infusion therapy in the treatment of NP were reviewed.
RESULTS
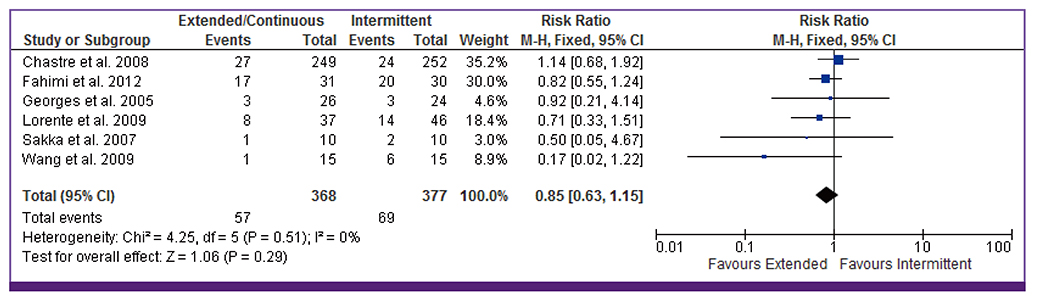
A total of ten studies were included in the analysis involving 1,051 cases of NP. Prolonged infusion of β-lactams was associated with higher clinical cure rate (OR 2.45, 95% CI, 1.12, 5.37) compared to intermittent infusion. However, there was no significant difference in mortality (OR 0.85, 95% CI 0.63-1.15) between the two groups. Subgroup analysis for β-lactam subclasses and for severity of illness showed comparable outcomes.
CONCLUSION
The limited data available suggest that reduced clinical failure rates when using prolonged infusions of β-lactam antibiotics in critically ill patients with NP. More detailed studies are needed to determine the impact of such strategy on mortality in this patient population.
Keyword
Figure
Cited by 1 articles
-
Prolonged or Continuous Infusion of IV Antibiotics as Initial Treatment Strategy
Hyuck Lee
Infect Chemother. 2016;48(2):140-142. doi: 10.3947/ic.2016.48.2.140.
Reference
-
1. Davis KA. Ventilator-associated pneumonia: a review. J Intensive Care Med. 2006; 21:211–226.
Article2. Safdar N, Dezfulian C, Collard HR, Saint S. Clinical and economic consequences of ventilator-associated pneumonia: a systematic review. Crit Care Med. 2005; 33:2184–2193.
Article3. Fagon JY, Chastre J, Hance AJ, Montravers P, Novara A, Gibert C. Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med. 1993; 94:281–288.
Article4. Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis. 1998; 26:1–10. quiz 11-2.
Article5. Kim MK, Capitano B, Mattoes HM, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP. Pharmacokinetic and pharmacodynamic evaluation of two dosing regimens for piperacillin-tazobactam. Pharmacotherapy. 2002; 22:569–577.
Article6. Kim MK, Xuan D, Quintiliani R, Nightingale CH, Nicolau DP. Pharmacokinetic and pharmacodynamic profile of high dose extended interval piperacillin-tazobactam. J Antimicrob Chemother. 2001; 48:259–267.
Article7. Burgess DS, Waldrep T. Pharmacokinetics and pharmacodynamics of piperacillin/tazobactam when administered by continuous infusion and intermittent dosing. Clin Ther. 2002; 24:1090–1104.
Article8. Roberts JA, Webb S, Paterson D, Ho KM, Lipman J. A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med. 2009; 37:2071–2078.
Article9. Tamma PD, Putcha N, Suh YD, Van Arendonk KJ, Rinke ML. Does prolonged beta-lactam infusions improve clinical outcomes compared to intermittent infusions? A meta-analysis and systematic review of randomized, controlled trials. BMC Infect Dis. 2011; 11:181.10. Mah GT, Mabasa VH, Chow I, Ensom MH. Evaluating outcomes associated with alternative dosing strategies for piperacillin/tazobactam: a qualitative systematic review. Ann Pharmacother. 2012; 46:265–275.
Article11. Deeks JJ, Dinnes J, D'Amico R, Sowden AJ, Sakarovitch C, Song F, Petticrew M, Altman DG. International Stroke Trial Collaborative Group. European Carotid Surgery Trial Collaborative Group. Evaluating non-randomised intervention studies. Health Technol Assess. 2003; 7:iii–x. 1–173.
Article12. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996; 17:1–12.
Article13. Hanes SD, Wood GC, Herring V, Croce MA, Fabian TC, Pritchard E, Boucher BA. Intermittent and continuous ceftazidime infusion for critically ill trauma patients. Am J Surg. 2000; 179:436–440.
Article14. McNabb JJ, Nightingale CH, Quintiliani R, Nicolau DP. Cost-effectiveness of ceftazidime by continuous infusion versus intermittent infusion for nosocomial pneumonia. Pharmacotherapy. 2001; 21:549–555.
Article15. Georges B, Conil JM, Cougot P, Decun JF, Archambaud M, Seguin T, Chabanon G, Virenque C, Houin G, Saivin S. Cefepime in critically ill patients: continuous infusion vs. an intermittent dosing regimen. Int J Clin Pharmacol Ther. 2005; 43:360–369.
Article16. Lorente L, Lorenzo L, Martin MM, Jimenez A, Mora ML. Meropenem by continuous versus intermittent infusion in ventilator-associated pneumonia due to gram-negative bacilli. Ann Pharmacother. 2006; 40:219–223.
Article17. Lorente L, Jiménez A, Palmero S, Jiménez JJ, Iribarren JL, Santana M, Martín MM, Mora ML. Comparison of clinical cure rates in adults with ventilator-associated pneumonia treated with intravenous ceftazidime administered by continuous or intermittent infusion: a retrospective, nonrandomized, open-label, historical chart review. Clin Ther. 2007; 29:2433–2439.
Article18. Lorente L, Jiménez A, Martín MM, Iribarren JL, Jiménez JJ, Mora ML. Clinical cure of ventilator-associated pneumonia treated with piperacillin/tazobactam administered by continuous or intermittent infusion. Int J Antimicrob Agents. 2009; 33:464–468.
Article19. Chastre J, Wunderink R, Prokocimer P, Lee M, Kaniga K, Friedland I. Efficacy and safety of intravenous infusion of doripenem versus imipenem in ventilator-associated pneumonia: a multicenter, randomized study. Crit Care Med. 2008; 36:1089–1096.
Article20. Wang D. Experience with extended-infusion meropenem in the management of ventilator-associated pneumonia due to multidrug-resistant Acinetobacter baumannii. Int J Antimicrob Agents. 2009; 33:290–291.
Article21. Sakka SG, Glauner AK, Bulitta JB, Kinzig-Schippers M, Pfister W, Drusano GL, Sörgel F. Population pharmacokinetics and pharmacodynamics of continuous versus short-term infusion of imipenem-cilastatin in critically ill patients in a randomized, controlled trial. Antimicrobial Agents Chemother. 2007; 51:3304–3310.
Article22. Fahimi F, Ghafari S, Jamaati H, Baniasadi S, Tabarsi P, Najafi A, Akhzarmehr A, Hashemian SM. Continuous versus intermittent administration of piperacillin-tazobactam in intensive care unit patients with ventilator-associated pneumonia. Indian J Crit Care Med. 2012; 16:141–147.
Article23. Lorente L, Leon C. [Femoral venous catheterization. Does it really need to be avoided?]. Med Intensiva. 2009; 33:442–449.24. Priest WS, Smith JM, McGEE CJ. The effect of anticoagulants on the penicillin therapy and the pathologic lesions of subacute bacterial endocarditis. N Engl J Med. 1946; 235:699–706.
Article25. Chant C, Leung A, Friedrich JO. Optimal dosing of antibiotics in critically ill patients by using continuous/extended infusions: a systematic review and meta-analysis. Crit Care. 2013; 17:R279.
Article26. Falagas ME, Tansarli GS, Ikawa K, Vardakas KZ. Clinical outcomes with extended or continuous versus short-term intravenous infusion of carbapenems and piperacillin/tazobactam: a systematic review and meta-analysis. Clin Infect Dis. 2013; 56:272–282.
Article27. Teo J, Liew Y, Lee W, Kwa AL. Prolonged infusion versus intermittent boluses of beta-lactam antibiotics for treatment of acute infections: a meta-analysis. Int J Antimicrob Agents. 2014; 43:403–411.
Article28. Shiu J, Wang E, Tejani AM, Wasdell M. Continuous versus intermittent infusions of antibiotics for the treatment of severe acute infections. Cochrane Database Syst Rev. 2013; 3:CD008481.
Article29. Kasiakou SK, Sermaides GJ, Michalopoulos A, Soteriades ES, Falagas ME. Continuous versus intermittent intravenous administration of antibiotics: a meta-analysis of randomised controlled trials. Lancet Infect Dis. 2005; 5:581–589.
Article30. Lodise TP, Lomaestro BM, Drusano GL. Society of Infectious Diseases Pharmacists. Application of antimicrobial pharmacodynamic concepts into clinical practice: focus on beta-lactam antibiotics: insights from the Society of Infectious Diseases Pharmacists. Pharmacotherapy. 2006; 26:1320–1332.
Article31. Jaruratanasirikul S, Sriwiriyajan S, Punyo J. Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother. 2005; 49:1337–1339.
Article32. De Jongh R, Hens R, Basma V, Mouton JW, Tulkens PM, Carryn S. Continuous versus intermittent infusion of temocillin, a directed spectrum penicillin for intensive care patients with nosocomial pneumonia: stability, compatibility, population pharmacokinetic studies and breakpoint selection. J Antimicrob Chemother. 2008; 61:382–388.
Article33. Boselli E, Breilh D, Rimmelé T, Poupelin JC, Saux MC, Chassard D, Allaouchiche B. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med. 2004; 30:989–991.
Article34. Chytra I, Stepan M, Benes J, Pelnar P, Zidkova A, Bergerova T, Pradl R, Kasal E. Clinical and microbiological efficacy of continuous versus intermittent application of meropenem in critically ill patients: a randomized open-label controlled trial. Crit Care. 2012; 16:R113.
Article35. Roberts JA, Boots R, Rickard CM, Thomas P, Quinn J, Roberts DM, Richards B, Lipman J. Is continuous infusion ceftriaxone better than once-a-day dosing in intensive care? A randomized controlled pilot study. J Antimicrob Chemother. 2007; 59:285–291.
Article36. Grant EM, Kuti JL, Nicolau DP, Nightingale C, Quintiliani R. Clinical efficacy and pharmacoeconomics of a continuous-infusion piperacillin-tazobactam program in a large community teaching hospital. Pharmacotherapy. 2002; 22:471–483.
Article37. Melsen WG, Rovers MM, Groenwold RH, Bergmans DC, Camus C, Bauer TT, Hanisch EW, Klarin B, Koeman M, Krueger WA, Lacherade JC, Lorente L, Memish ZA, Morrow LE, Nardi G, van Nieuwenhoven CA, O'Keefe GE, Nakos G, Scannapieco FA, Seguin P, Staudinger T, Topeli A, Ferrer M, Bonten MJ. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013; 13:665–671.
Article38. Lodise TP Jr, Lomaestro B, Drusano GL. Piperacillin-tazobactam for Pseudomonas aeruginosa infection: clinical implications of an extended-infusion dosing strategy. Clin Infect Dis. 2007; 44:357–363.
Article39. Boselli E, Breilh D, Rimmele T, Guillaume C, Xuereb F, Saux MC, Bouvet L, Chassard D, Allaouchiche B. Alveolar concentrations of piperacillintazobactam administered in continuous infusion to patients with ventilator-associated pneumonia. Crit Care Med. 2008; 36:1500–1506.
Article40. Felton TW, Goodwin J, O'Connor L, Sharp A, Gregson L, Livermore J, Howard SJ, Neely MN, Hope WW. Impact of Bolus dosing versus continuous infusion of Piperacillin and Tazobactam on the development of antimicrobial resistance in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013; 57:5811–5819.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Gastric pH on the Nosocomial Pneumonia in Long - term Intubated Patients
- Some Effects of Histamine Type 2 Blockers on the Nosocomial Pneumonia in Patients with Prolonged Intubation
- Continuous infusion versus intermittent bolus injection of propofol during endoscopic retrograde cholangiopancreatography
- Nosocomial Pseudomonas putida Bacteremia: High Rates of Carbapenem Resistance and Mortality
- Is β-Lactam Plus Macrolide More Effective than β-Lactam Plus Fluoroquinolone among Patients with Severe Community-Acquired Pneumonia?: a Systemic Review and Meta-Analysis