J Korean Soc Radiol.
2016 Jul;75(1):17-25. 10.3348/jksr.2016.75.1.17.
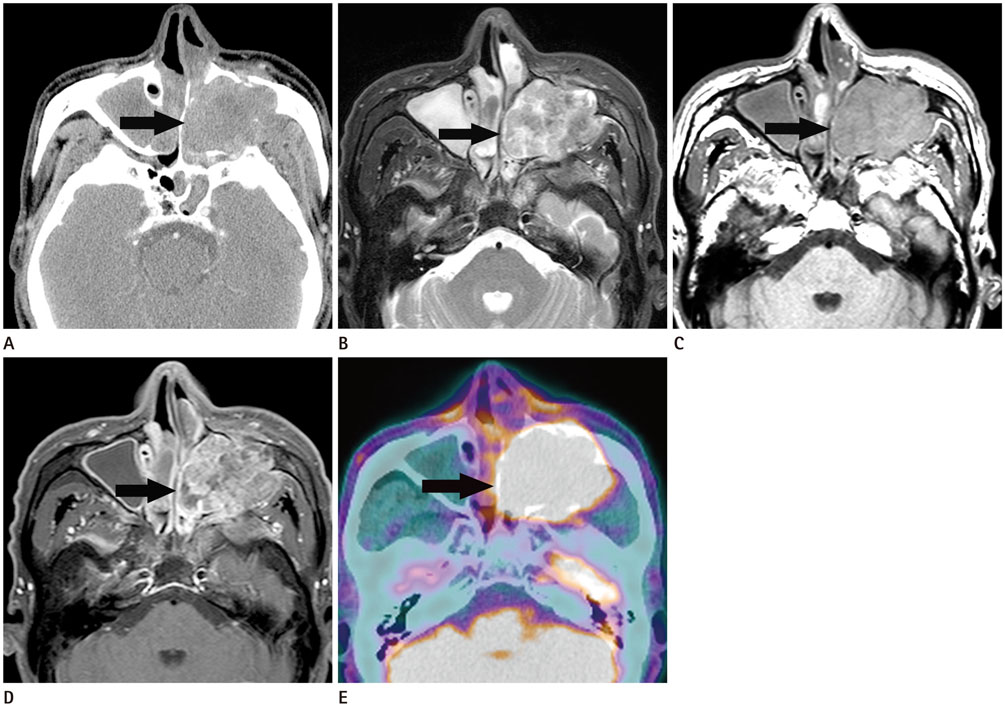
CT, MRI, and FDG PET/CT Findings of Sinonasal Sarcoma: Differentiation from Squamous Cell Carcinoma
- Affiliations
-
- 1Department of Radiology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. evee0914@chollian.net
- 2Department of Nuclear Medicine, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Ilsong Memorial Institute of Head and Neck Cancer, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
- KMID: 2327362
- DOI: http://doi.org/10.3348/jksr.2016.75.1.17
Abstract
- PURPOSE
To evaluate computed tomography (CT), magnetic resonance imaging (MRI), and 18F-fluorodeoxyglucose (FDG) positron emission tomography/CT (PET/CT) findings for the differentiation of sinonasal sarcoma from squamous cell carcinoma (SCC).
MATERIALS AND METHODS
We retrospectively reviewed CT, MRI, and FDG PET/CT results in 20 patients with pathologically proven sinonasal sarcoma (n = 7) and SCC (n = 13). Imaging characteristics of tumors, such as the shape, size, margin, MRI signal intensity, pattern of enhancement, local tumor invasion, and maximum standardized uptake value (SUVmax) were analyzed and compared between sarcoma and SCC.
RESULTS
The SUVmax of sarcomas (7.4 ± 2.1) was significantly lower than the SUVmax of the SCCs (14.3 ± 4.5) (p = 0.0013). However, no significant difference in the shape, size, margin, MRI signal intensity, pattern of enhancement, and local tumor invasion was observed between sarcoma and SCC.
CONCLUSION
Although CT and MR imaging features are nonspecific, FDG PET/CT is useful in distinguishing between sinonasal sarcoma and SCC based on the SUVmax value.
MeSH Terms
Figure
Reference
-
1. Figueiredo MT, Marques LA, Campos-Filho N. Soft-tissue sarcomas of the head and neck in adults and children: experience at a single institution with a review of literature. Int J Cancer. 1988; 41:198–200.2. Gorsky M, Epstein JB. Head and neck and intra-oral soft tissue sarcomas. Oral Oncol. 1998; 34:292–296.3. Wanebo HJ, Koness RJ, MacFarlane JK, Eilber FR, Byers RM, Elias EG, et al. Head and neck sarcoma: report of the Head and Neck Sarcoma Registry. Society of Head and Neck Surgeons Committee on Research. Head Neck. 1992; 14:1–7.4. Madani G, Beale TJ, Lund VJ. Imaging of sinonasal tumors. Semin Ultrasound CT MR. 2009; 30:25–38.5. Dooley L, Shah J. Management of the neck in maxillary sinus carcinomas. Curr Opin Otolaryngol Head Neck Surg. 2015; 23:107–114.6. Sercarz JA, Mark RJ, Tran L, Storper I, Calcaterra TC. Sarcomas of the nasal cavity and paranasal sinuses. Ann Otol Rhinol Laryngol. 1994; 103:699–704.7. Patel SG, Shah JP. TNM staging of cancers of the head and neck: striving for uniformity among diversity. CA Cancer J Clin. 2005; 55:242–258. quiz 261-262, 264.8. Sakai O, Curtin HD, Romo LV, Som PM. Lymph node pathology. Benign proliferative, lymphoma, and metastatic disease. Radiol Clin North Am. 2000; 38:979–998. x9. Lee HN, Han JK, Kim HH, Shin HC, Kim IY, Jou SS. Comparative study of lymph node metastasis from squamous cell carcinoma and non-squamous cell carcinoma on neck CT. Korean Soc Radiol. 2015; 72:271–281.10. Arnold A, Ziglinas P, Ochs K, Alter N, Geretschläger A, Lädrach K, et al. Therapy options and long-term results of sinonasal malignancies. Oral Oncol. 2012; 48:1031–1037.11. Weber AL, Stanton AC. Malignant tumors of the paranasal sinuses: radiologic, clinical, and histopathologic evaluation of 200 cases. Head Neck Surg. 1984; 6:761–776.12. Sanghvi S, Khan MN, Patel NR, Yeldandi S, Baredes S, Eloy JA. Epidemiology of sinonasal squamous cell carcinoma: a comprehensive analysis of 4994 patients. Laryngoscope. 2014; 124:76–83.13. Lin M, Shon IH, Lin P. Positron emission tomography: current status and future challenges. Intern Med J. 2010; 40:19–29.14. Som PM, Brandwein MS. Tumors and tumor-like conditions. In : Som PM, Curtin DC, editors. Head and neck imaging. St. Louis: Mosby;2003. p. 261–373.15. Lloyd GA, Phelps PD, Michaels L. The imaging characteristics of naso-sinus chondrosarcoma. Clin Radiol. 1992; 46:189–192.16. Park SW, Kim HJ, Lee JH, Ko YH. Malignant fibrous histiocytoma of the head and neck: CT and MR imaging findings. AJNR Am J Neuroradiol. 2009; 30:71–76.17. Benz MR, Dry SM, Eilber FC, Allen-Auerbach MS, Tap WD, Elashoff D, et al. Correlation between glycolytic phenotype and tumor grade in soft-tissue sarcomas by 18F-FDG PET. J Nucl Med. 2010; 51:1174–1181.18. Charest M, Hickeson M, Lisbona R, Novales-Diaz JA, Derbekyan V, Turcotte RE. FDG PET/CT imaging in primary osseous and soft tissue sarcomas: a retrospective review of 212 cases. Eur J Nucl Med Mol Imaging. 2009; 36:1944–1951.19. Israel-Mardirosian N, Adler LP. Positron emission tomography of soft tissue sarcomas. Curr Opin Oncol. 2003; 15:327–330.20. Ioannidis JP, Lau J. 18F-FDG PET for the diagnosis and grading of soft-tissue sarcoma: a meta-analysis. J Nucl Med. 2003; 44:717–724.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Role of F-18 FDG PET/CT in Squamous Cell Carcinoma of Head and Neck
- Recurrent Follicular Dendritic Cell Sarcoma of the Parotid Gland Imaged with 18F-FDG PET/CT
- Accuracy of F-18 FDG PET/CT in Preoperative Assessment of Cervical Lymph Nodes in Head and Neck Squamous Cell Cancer: Comparison with CT/MRI
- F-18 FDG PET/CT Finding in Solid Pseudo-papillary Tumor of the Pancreas 6 years After Initial Diagnosis
- Multiple Skeletal Muscle Metastases in a Case of Transitional Cell Carcinoma of Bladder Detected by F-18 FDG PET/CT