J Korean Soc Radiol.
2016 Jul;75(1):1-11. 10.3348/jksr.2016.75.1.1.
CT Findings of Benign Omental Lesions Following Abdominal Cancer Surgery
- Affiliations
-
- 1Department of Diagnostic Radiology, Dong-A University College of Medicine, Busan, Korea. ohjy@dau.ac.kr
- KMID: 2327360
- DOI: http://doi.org/10.3348/jksr.2016.75.1.1
Abstract
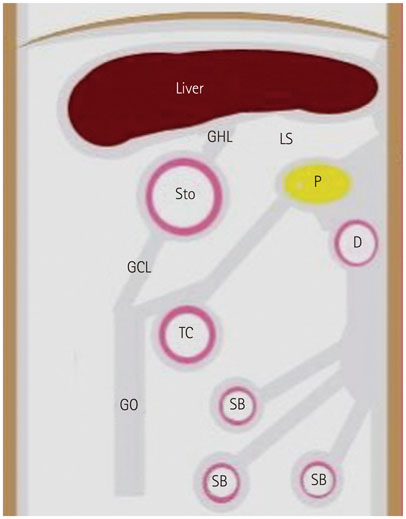
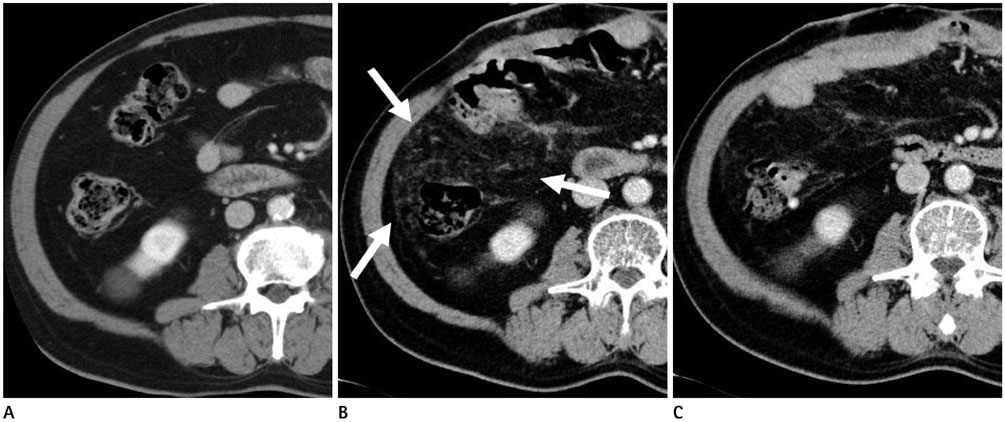
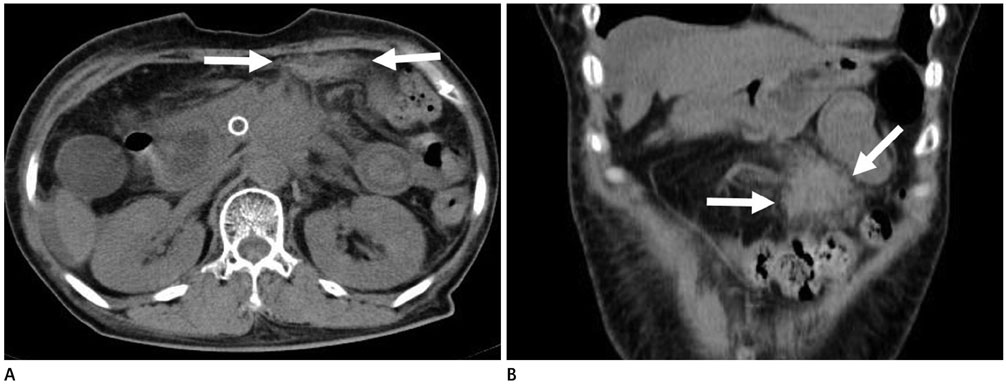
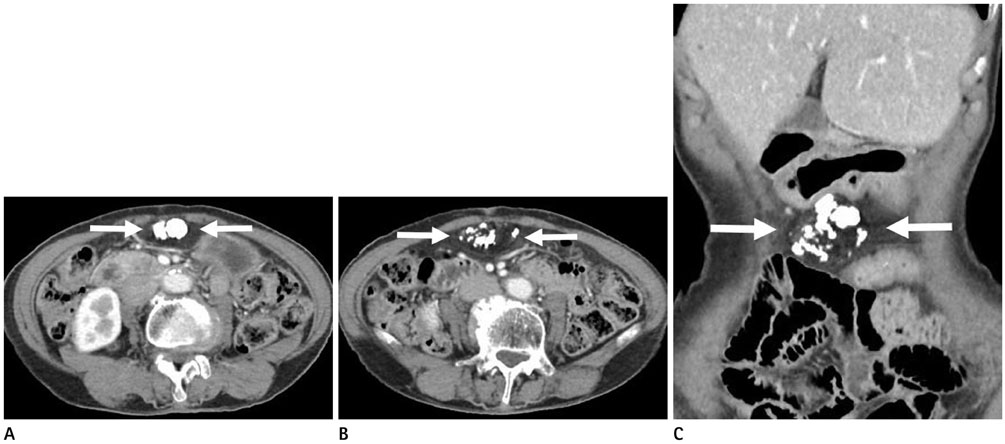
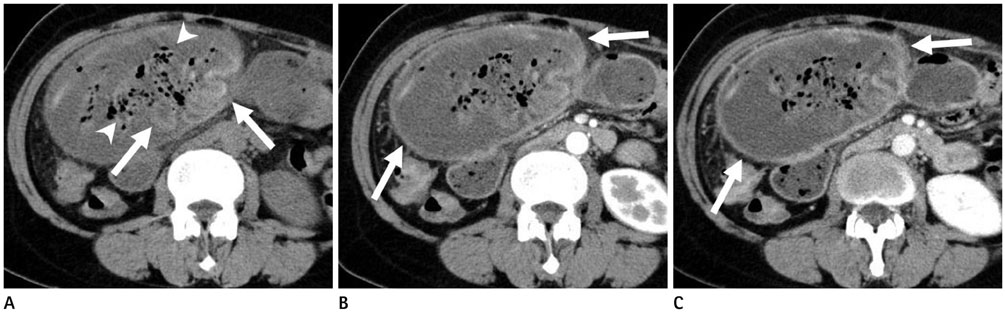
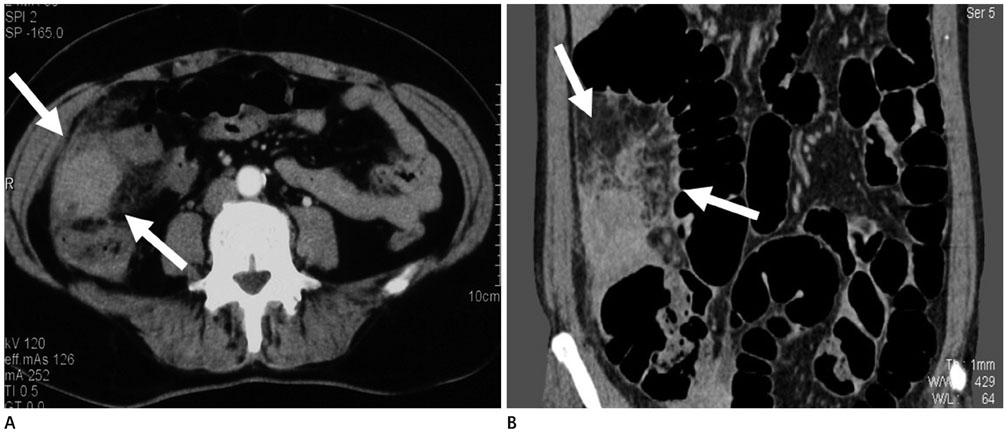
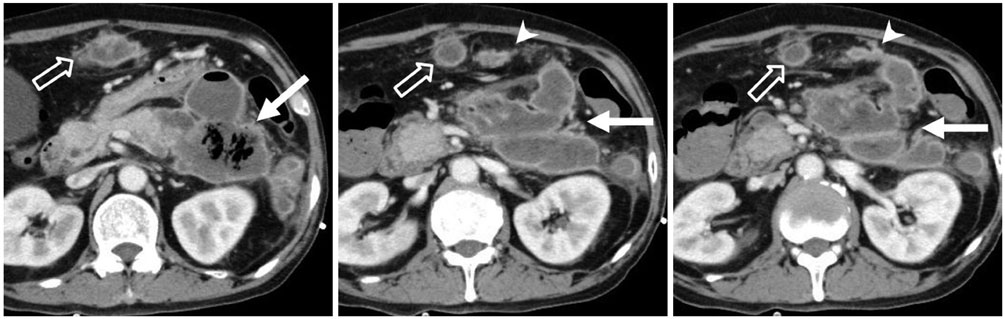
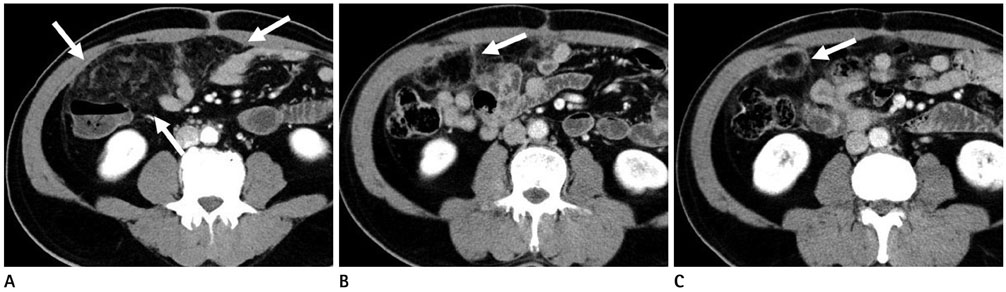
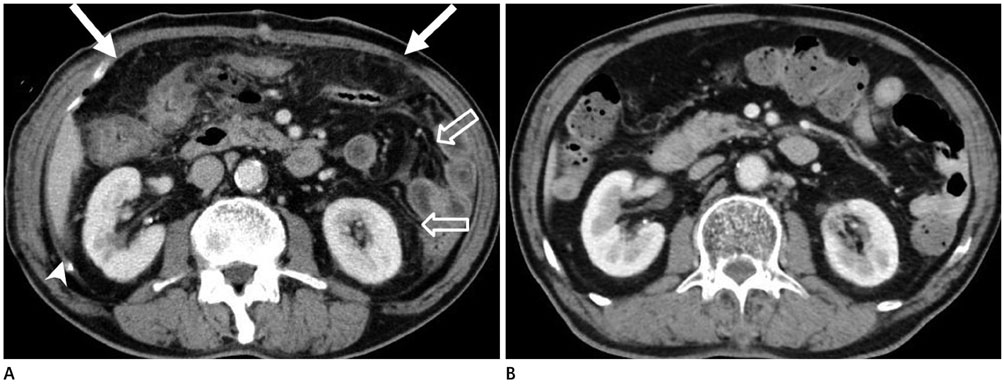
- The greater omentum is the largest peritoneal fold and can be the origin of primary pathologic conditions, as well as a boundary and conduit for disease processes. Most diseases involving the omentum manifest with nonspecific and overlapping features on computed tomography (CT). In particular, varying benign disease processes of traumatic, inflammatory, vascular, or systemic origin can occur in the omentum during the follow-up period after surgery for intra-abdominal malignancy. It can be challenging for radiologists due to various spectrum of CT findings. Thus, we reviewed the CT findings of various benign omental lesions after surgery for intra-abdominal malignancy.
MeSH Terms
Figure
Cited by 2 articles
-
Omental Infarction Associated with Rib Cage Anomaly in Achondroplasia: Report of a Rare Case
Tae Hyung Kim, You Sung Kim
J Korean Soc Radiol. 2019;80(5):992-996. doi: 10.3348/jksr.2019.80.5.992.Omental Torsion and Infarction with Right Inguinal Hernia: A Case Report
You Sung Kim, Tae Hyung Kim
J Korean Soc Radiol. 2017;77(3):183-186. doi: 10.3348/jksr.2017.77.3.183.
Reference
-
1. Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet. 2000; 70:209–226.2. Kodera Y, Nakanishi H, Ito S, Yamamura Y, Kanemitsu Y, Shimizu Y, et al. Quantitative detection of disseminated cancer cells in the greater omentum of gastric carcinoma patients with real-time RT-PCR: a comparison with peritoneal lavage cytology. Gastric Cancer. 2002; 5:69–76.3. Deraco M, Santoro N, Carraro O, Inglese MG, Rebuffoni G, Guadagni S, et al. Peritoneal carcinomatosis: feature of dissemination. A review. Tumori. 1999; 85:1–5.4. Bosch B, Guller U, Schnider A, Maurer R, Harder F, Metzger U, et al. Perioperative detection of disseminated tumour cells is an independent prognostic factor in patients with colorectal cancer. Br J Surg. 2003; 90:882–888.5. Kim MC, Kim KH, Jung GJ, Rattner DW. Comparative study of complete and partial omentectomy in radical subtotal gastrectomy for early gastric cancer. Yonsei Med J. 2011; 52:961–966.6. Ha TK, An JY, Youn HG, Noh JH, Sohn TS, Kim S. Omentum-preserving gastrectomy for early gastric cancer. World J Surg. 2008; 32:1703–1708.7. Hasegawa S, Kunisaki C, Ono H, Oshima T, Fujii S, Taguri M, et al. Omentum-preserving gastrectomy for advanced gastric cancer: a propensity-matched retrospective cohort study. Gastric Cancer. 2013; 16:383–388.8. Moore KL. The developing human: clinically oriented embryology. Philadelphia: Saunders;1982. p. 227–229.9. Sompayrac SW, Mindelzun RE, Silverman PM, Sze R. The greater omentum. AJR Am J Roentgenol. 1997; 168:683–687.10. Collins D, Hogan AM, O'Shea D, Winter DC. The omentum: anatomical, metabolic, and surgical aspects. J Gastrointest Surg. 2009; 13:1138–1146.11. Singh AK, Gervais DA, Lee P, Westra S, Hahn PF, Novelline RA, et al. Omental infarct: CT imaging features. Abdom Imaging. 2006; 31:549–554.12. Rossi A, Rossi G. CT of the peritoneum. Berlin: Springer;2001. p. 217.13. Ghiatas AA, Fisher R. CT of spontaneous haematoma of the omentum. Eur Radiol. 1994; 4:474–475.14. Bhandari RS, Sapkota R, Mishra P, Singh KP. Spontaneous omental hematoma. J Inst Med. 2009; 31:20–22.15. Shi X, Zhang W, Nabieu PF, Zhao W, Fu C. Early postoperative heterotopic omental ossification: report of a case. Surg Today. 2011; 41:137–140.16. Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004; 12:116–125.17. Myers MA, Minton JP. Heterotopic ossification within the small-bowel mesentery. Arch Surg. 1989; 124:982–983.18. Lai HJ, Jao SW, Lee TY, Ou JJ, Kang JC. Heterotopic mesenteric ossification after total colectomy for bleeding diverticulosis of the colon--a rare case report. J Formos Med Assoc. 2007; 106:2 Suppl. S32–S36.19. Jacobs JE, Birnbaum BA, Siegelman ES. Heterotopic ossification of midline abdominal incisions: CT and MR imaging findings. AJR Am J Roentgenol. 1996; 166:579–584.20. Kim KW, Choi BI, Han JK, Kim TK, Kim AY, Lee HJ, et al. Postoperative anatomic and pathologic findings at CT following gastrectomy. Radiographics. 2002; 22:323–336.21. Balthazar EJ, Lefkowitz RA. Left-sided omental infarction with associated omental abscess: CT diagnosis. J Comput Assist Tomogr. 1993; 17:379–381.22. Williams RG, Bragg DG, Nelson JA. Gossypiboma--the problem of the retained surgical sponge. Radiology. 1978; 129:323–326.23. Manzella A, Filho PB, Albuquerque E, Farias F, Kaercher J. Imaging of gossypibomas: pictorial review. AJR Am J Roentgenol. 2009; 193:6 Suppl. S94–S101.24. Choi BI, Kim SH, Yu ES, Chung HS, Han MC, Kim CW. Retained surgical sponge: diagnosis with CT and sonography. AJR Am J Roentgenol. 1988; 150:1047–1050.25. Ribalta T, McCutcheon IE, Neto AG, Gupta D, Kumar AJ, Biddle DA, et al. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Arch Pathol Lab Med. 2004; 128:749–758.26. Apter S, Hertz M, Rubinstein ZJ, Zissin R. Gossypiboma in the early post-operative period: a diagnostic problem. Clin Radiol. 1990; 42:128–129.27. Topal U, Gebitekin C, Tuncel E. Intrathoracic gossypiboma. AJR Am J Roentgenol. 2001; 177:1485–1486.28. Lu YY, Cheung YC, Ko SF, Ng SH. Calcified reticulate rind sign: a characteristic feature of gossypiboma on computed tomography. World J Gastroenterol. 2005; 11:4927–4929.29. Sabaté JM, Torrubia S, Maideu J, Franquet T, Monill JM, Pérez C. Sclerosing mesenteritis: imaging findings in 17 patients. AJR Am J Roentgenol. 1999; 172:625–629.30. Daskalogiannaki M, Voloudaki A, Prassopoulos P, Magkanas E, Stefanaki K, Apostolaki E, et al. CT evaluation of mesenteric panniculitis: prevalence and associated diseases. AJR Am J Roentgenol. 2000; 174:427–431.31. Katz ME, Heiken JP, Glazer HS, Lee JK. Intraabdominal panniculitis: clinical, radiographic, and CT features. AJR Am J Roentgenol. 1985; 145:293–296.32. Jeon EJ, Cho SM. Idiopathic isolated omental panniculitis confirmed by percutaneous CT-guided biopsy. Gut Liver. 2009; 3:321–324.33. Rozin A, Bishara B, Ben-Izhak O, Fischer D, Carter A, Edoute Y. Fibrosing omental panniculitis and polyserositis associated with long-term treatment by paroxetine. Isr Med Assoc J. 2000; 2:714–716.34. Hirono S, Sakaguchi S, Iwakura S, Masaki K, Tsuhada K, Yamaue H. Idiopathic isolated omental panniculitis. J Clin Gastroenterol. 2005; 39:79–80.35. Lheureux P, Matos C, Charlier PH, Van Romphey A, Rickaert F, Van Gansbeke D, et al. Omental panniculitis: an unusual cause of acute appendiceal syndrome. Ann Emerg Med. 1987; 16:224–226.36. Horton KM, Lawler LP, Fishman EK. CT findings in sclerosing mesenteritis (panniculitis): spectrum of disease. Radiographics. 2003; 23:1561–1567.37. van Breda Vriesman AC, Schuttevaer HM, Coerkamp EG, Puylaert JB. Mesenteric panniculitis: US and CT features. Eur Radiol. 2004; 14:2242–2248.38. Kuo IM, Wang F, Liu KH, Jan YY. Post-gastrectomy acute pancreatitis in a patient with gastric carcinoma and pancreas divisum. World J Gastroenterol. 2009; 15:4596–4600.39. Choi BI. Radiology illustrated: gastrointestinal tract. Berlin: Springer;2014. p. 222.40. Soybel DI, Zinner MJ. Complications following gastric operations. In : Zinner MJ, Schwartz SI, editors. Maingot's abdominal operations. Stamford, CT: Appleton and Lange;1997. p. 1029–1056.41. Doglietto GB, Pacelli F, Caprino P, Bossola M, Di Stasi C. Pancreas-preserving total gastrectomy for gastric cancer. Arch Surg. 2000; 135:89–94.42. Mindelzun RE, Jeffrey RB Jr, Lane MJ, Silverman PM. The misty mesentery on CT: differential diagnosis. AJR Am J Roentgenol. 1996; 167:61–65.43. Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology. 2012; 262:751–764.44. Hamrick-Turner JE, Chiechi MV, Abbitt PL, Ros PR. Neoplastic and inflammatory processes of the peritoneum, omentum, and mesentery: diagnosis with CT. Radiographics. 1992; 12:1051–1068.45. Leitner MJ, Jordan CG, Spinner MH, Reese EC. Torsion, infarction and hemorrhage of the omentum as a cause of acute abdominal distress. Ann Surg. 1952; 135:103–110.46. Naffaa LN, Shabb NS, Haddad MC. CT findings of omental torsion and infarction: case report and review of the literature. Clin Imaging. 2003; 27:116–118.47. Kim J, Kim Y, Cho OK, Rhim H, Koh BH, Kim YS, et al. Omental torsion: CT features. Abdom Imaging. 2004; 29:502–504.48. Stella DL, Schelleman TG. Segmental infarction of the omentum secondary to torsion: ultrasound and computed tomography diagnosis. Australas Radiol. 2000; 44:212–215.49. Schwartzman GJ, Jacobs JE, Birnbaum BA. Omental infarction as a delayed complication of abdominal surgery. Clin Imaging. 2001; 25:341–343.50. Dallal RM, Bailey LA. Omental infarction: a cause of acute abdominal pain after antecolic gastric bypass. Surg Obes Relat Dis. 2006; 2:451–454.51. Bestman TJ, Valk JW, Gypen B, Declercq S, Hendrickx L. An unusual complication after Roux-en-Y gastric bypass: torsion and infarction of the divided Omentum. Obes Surg. 2009; 19:1731–1733.52. Oh JY, Cho JH, Kang MJ, Lee JH, Kwon HJ, Nam KJ, et al. Omental infarction caused by laparoscopy-assisted gastrectomy for gastric cancer: CT findings. Clin Radiol. 2011; 66:966–973.53. Yoo E, Kim JH, Kim MJ, Yu JS, Chung JJ, Yoo HS, et al. Greater and lesser omenta: normal anatomy and pathologic processes. Radiographics. 2007; 27:707–720.54. Tyrrel RT, Montemayor KA, Bernardino ME. CT density of mesenteric, retroperitoneal, and subcutaneous fat in cirrhotic patients: comparison with control subjects. AJR Am J Roentgenol. 1990; 155:73–75.55. Chopra S, Dodd GD 3rd, Chintapalli KN, Esola CC, Ghiatas AA. Mesenteric, omental, and retroperitoneal edema in cirrhosis: frequency and spectrum of CT findings. Radiology. 1999; 211:737–742.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Omental Infarction Following Laparoscopy-assisted Gastrectomy (LAG) for Gastric Cancer
- Idiopathic Omental Infarction to Be a Rare Cause of Acute Abdomen: A Case Report
- Omental Cyst
- Omental Infarction Associated with Rib Cage Anomaly in Achondroplasia: Report of a Rare Case
- Computed Tomography and Ultrasound of Omental Infarction in Children: Differential Diagnoses of Right Lower Quadrant Pain