J Korean Soc Radiol.
2019 Sep;80(5):992-996. 10.3348/jksr.2019.80.5.992.
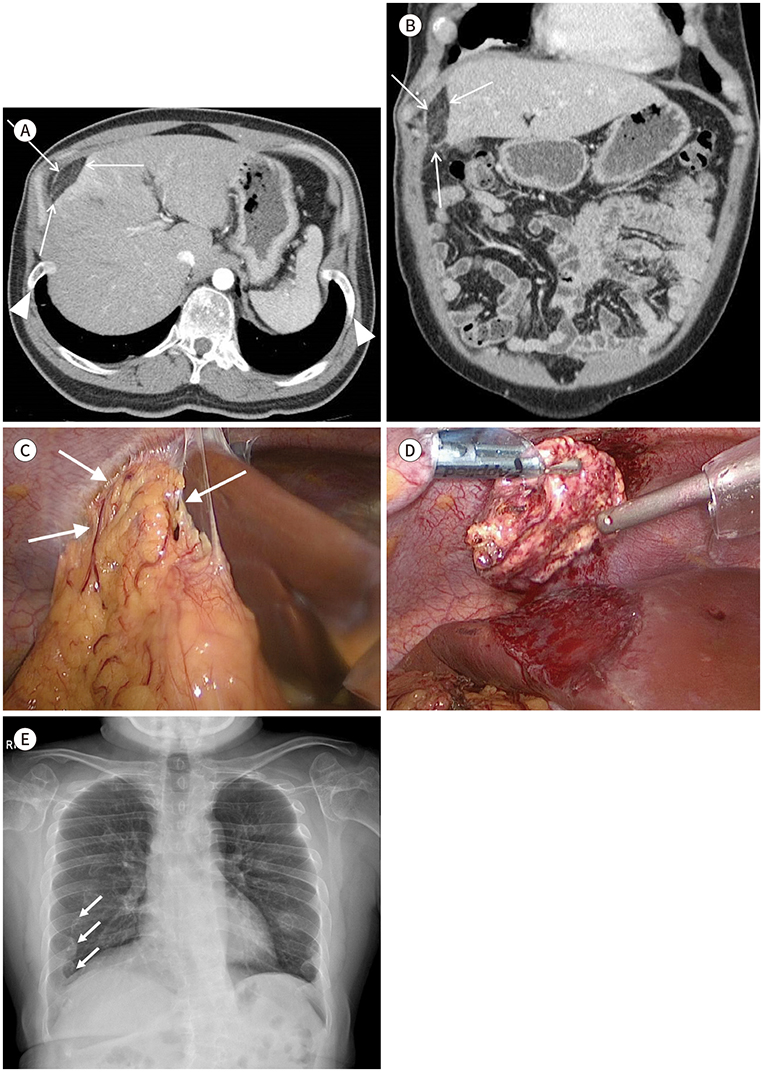
Omental Infarction Associated with Rib Cage Anomaly in Achondroplasia: Report of a Rare Case
- Affiliations
-
- 1Department of Radiology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. youskim@gmail.com
- KMID: 2459027
- DOI: http://doi.org/10.3348/jksr.2019.80.5.992
Abstract
- Omental infarction, a rare cause of acute abdominal pain, is usually difficult to diagnose before surgery. Several studies have shown that CT is useful in diagnosing an omental infarction. We report the first case of an omental infarction secondary to rib cage anomaly associated with achondroplasia. Preoperative CT revealed a fatty mass in the anterior perihepatic space and anterior flaring of the ribs. The patient, a 41-year-old man, was diagnosed with omental infarction in the anterior perihepatic space and treated with intravenous painkillers. After discharge, because of recurrent abdominal pain, he was readmitted and successfully underwent laparoscopic partial omentectomy. The mass was confirmed to be an infarcted omentum with fat necrosis and hemorrhage. Thus, omental infarction should be considered as a differential diagnosis for acute abdominal pain, especially in patients with achondroplasia. Contrast-enhanced abdominal CT can help in correctly diagnosing a suspected omental infarction.
MeSH Terms
Figure
Reference
-
1. Grattan-Smith JD, Blews DE, Brand T. Omental infarction in pediatric patients: sonographic and CT findings. AJR Am J Roentgenol. 2002; 178:1537–1539.
Article2. Singh AK, Gervais DA, Hahn PF, Sagar P, Mueller PR, Novelline RA. Acute epiploic appendagitis and its mimics. Radiographics. 2005; 25:1521–1534.
Article3. Horton WA, Hall JG, Hecht JT. Achondroplasia. Lancet. 2007; 370:162–172.
Article4. Glass RB, Norton KI, Mitre SA, Kang E. Pediatric ribs: a spectrum of abnormalities. Radiographics. 2002; 22:87–104.
Article5. Park KE, Chung DJ, Kim W, Hahn ST, Lee JM. Secondary omental infarction related to open and laparoscopic-assisted distal gastrectomy: report of two cases. Korean J Radiol. 2011; 12:757–760.
Article6. Lee SY, Kim DW, Cho JH, Kwon HJ, Ha DH, Oh JY. CT findings of benign omental lesions following abdominal cancer surgery. J Korean Soc Radiol. 2016; 75:1–11.
Article7. Park TU, Oh JH, Chang IT, Lee SJ, Kim SE, Kim CW, et al. Omental infarction: case series and review of the literature. J Emerg Med. 2012; 42:149–154.
Article8. Kim YS, Kim TH. Omental torsion and infarction with right inguinal hernia: a case report. J Korean Soc Radiol. 2017; 77:183–186.
Article9. Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol (N Y). 2012; 8:276–227.10. Nubi A, McBride W, Stringel G. Primary omental infarct: conservative vs operative management in the era of ultrasound, computerized tomography, and laparoscopy. J Pediatr Surg. 2009; 44:953–956.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Omental Infarction to Be a Rare Cause of Acute Abdomen: A Case Report
- Omental Torsion and Infarction with Right Inguinal Hernia: A Case Report
- CT Findings of Primary Torsion of the Greater Omentum with Segmental Infarction: Case Report
- Thoracic Myelopathy due to Thoracolumbar Kyphosis and Spinal Stenosis in Achondroplasia: A Case Report
- A case of torsion of an omental leiomyoma misdiagnosed as torsion of an adnexal mass