J Korean Surg Soc.
2013 Nov;85(5):199-204.
Antiadhesive effect and safety of sodium hyaluronate-carboxymethyl cellulose membrane in thyroid surgery
- Affiliations
-
- 1Department of Surgery, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Department of Surgery, Seoul National University Hospital, Seoul, Korea. kyu.eun.lee.md@gmail.com
- 3Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
Abstract
- PURPOSE
A number of researchers have suggested the use of sodium hyaluronate carboxymethyl cellulose (HA-CMC) membrane for preventing postoperative adhesion. This study evaluated the antiadhesive effect and safety of HA-CMC membrane in thyroidectomy for papillary thyroid cancer.
METHODS
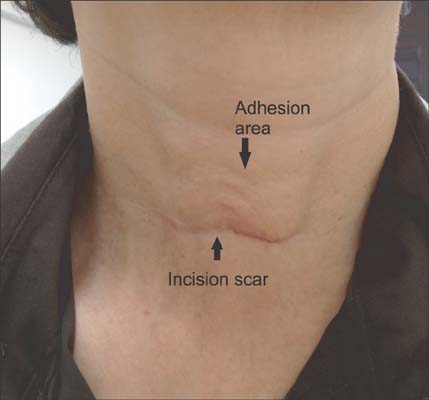
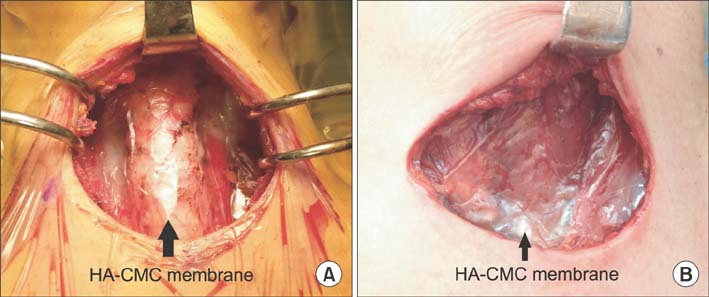
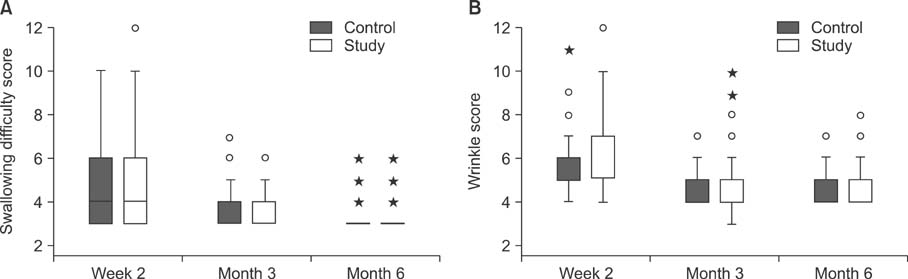
One hundred sixty-two patients who underwent thyroidectomy were prospectively randomized. In the study group of 80 patients, the 7.5 cm x 13 cm HA-CMC membrane was applied to the operative field after thyroidectomy. The subjects were asked about complications including adhesive symptoms using an 8-item questionnaire at 2 weeks, 3 months, and 6 months after surgery. In addition, items on the appearance of neck wrinkles and scars were evaluated by a physician who had no information about the patient's allocation.
RESULTS
There were no significant differences in complications such as swallowing difficulty, and wrinkles between study and control groups. Both groups presented significantly decreased scores over time in swallowing difficulty, and wrinkles. There were no complications regarding the HA-CMC membrane.
CONCLUSION
The antiadhesive effect of HA-CMC membrane in thyroid surgery is still uncertain, although it is biologically safe. Further investigation is needed to confirm the antiadhesive effect of HA-CMC membrane in thyroid surgery.
MeSH Terms
Figure
Reference
-
1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Seo HG, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat. 2012; 44:11–24.2. Park WS, Chung YS, Lee KE, Kim HY, Choe JH, Koh SH, et al. Anti-adhesive effect and safety of sodium hyaluronate and sodium carboxymethyl cellulose solution in thyroid surgery. Asian J Surg. 2010; 33:25–30.3. Becker JM, Dayton MT, Fazio VW, Beck DE, Stryker SJ, Wexner SD, et al. Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized, double-blind multicenter study. J Am Coll Surg. 1996; 183:297–306.4. Fazio VW, Cohen Z, Fleshman JW, van Goor H, Bauer JJ, Wolff BG, et al. Reduction in adhesive small-bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006; 49:1–11.5. Kutlay J, Ozer Y, Isik B, Kargici H. Comparative effectiveness of several agents for preventing postoperative adhesions. World J Surg. 2004; 28:662–665.6. Metwally M, Cheong Y, Li TC. A review of techniques for adhesion prevention after gynaecological surgery. Curr Opin Obstet Gynecol. 2008; 20:345–352.7. Kusunoki M, Ikeuchi H, Yanagi H, Noda M, Tonouchi H, Mohri Y, et al. Bioresorbable hyaluronate-carboxymethylcellulose membrane (Seprafilm) in surgery for rectal carcinoma: a prospective randomized clinical trial. Surg Today. 2005; 35:940–945.8. Zeng Q, Yu Z, You J, Zhang Q. Efficacy and safety of Seprafilm for preventing postoperative abdominal adhesion: systematic review and meta-analysis. World J Surg. 2007; 31:2125–2131.9. Yigit O, Uslu Coskun B, Coskun H, Yilmaz B, Alkan S, Cinar U, et al. Efficacy of anti-adhesive barriers in secondary thy ro idectomy: an experimental study. Laryngoscope. 2004; 114:1668–1673.10. Osada H, Minai M, Tsunoda I, Fujii TK, Tsubata K, Satoh K. The effect of hyaluronic acid-carboxymethylcellulose in reducing adhesion reformation in rabbits. J Int Med Res. 1999; 27:292–296.11. Baakdah H, Tulandi T. Adhesion in gynecology complication, cost, and prevention: a review. Surg Technol Int. 2005; 14:185–190.12. Parker MC, Wilson MS, Menzies D, Sunderland G, Thompson JN, Clark DN, et al. Colorectal surgery: the risk and burden of adhesion-related complications. Colorectal Dis. 2004; 6:506–511.13. Menzies D. Peritoneal adhesions. Incidence, cause, and prevention. Surg Annu. 1992; 24 Pt 1:27–45.14. Divilio LT. Surgical adhesion development and prevention. Int Surg. 2005; 90:3 Suppl. S6–S9.15. Greenawalt KE, Corazzini RL, Colt MJ, Holmdahl L. Adhesion formation to hemostatic agents and its reduction with a sodium hyaluronate/carboxymethylcellulose adhesion barrier. J Biomed Mater Res A. 2012; 100:1777–1782.16. Yang EJ, Kang E, Jang JY, Kim D, Yom CK, Lim JY, et al. Effect of a mixed solution of sodium hyaluronate and carboxymethyl cellulose on upper limb dysfunction after total mastectomy: a double-blind, randomized clinical trial. Breast Cancer Res Treat. 2012; 136:187–194.17. Bristow RE, Montz FJ. Prevention of adhesion formation after radical oophorectomy using a sodium hyaluronate-carboxymethylcellulose (HA-CMC) barrier. Gynecol Oncol. 2005; 99:301–308.18. Mumert ML, Altay T, Couldwell WT. Technique for decompressive craniectomy using Seprafilm as a dural substitute and anti-adhesion barrier. J Clin Neurosci. 2012; 19:455–457.19. Ahn JH, Lim HW, Hong HR. The clinical application and efficacy of sodium hyaluronate-carboxymethylcellulose during tympanomastoid surgery. Laryngoscope. 2012; 122:912–915.20. Hashimoto D, Hirota M, Yagi Y, Baba H. Hyaluronate carboxymethylcellulose-based bioresorbable membrane (Seprafilm) reduces adhesion under the incision to make unplanned relaparotomy safer. Surg Today. 2012; 42:863–867.21. Sheldon HK, Gainsbury ML, Cassidy MR, Chu DI, Stucchi AF, Becker JM. A sprayable hyaluronate/carboxymethylcellulose adhesion barrier exhibits regional adhesion reduction efficacy and does not impair intestinal healing. J Gastrointest Surg. 2012; 16:325–333.22. Krill LS, Ueda SM, Gerardi M, Bristow RE. Analysis of postoperative complications associated with the use of anti-adhesion sodium hyaluronate-carboxymethylcellulose (HA-CMC) barrier after cytoreductive surgery for ovarian, fallopian tube and peritoneal cancers. Gynecol Oncol. 2011; 120:220–223.23. Lalountas M, Ballas KD, Michalakis A, Psarras K, Asteriou C, Giakoustidis DE, et al. Postoperative adhesion prevention using a statin-containing cellulose film in an experimental model. Br J Surg. 2012; 99:423–429.24. Lalountas MA, Ballas KD, Skouras C, Asteriou C, Kontoulis T, Pissas D, et al. Preventing intraperitoneal adhesions with atorvastatin and sodium hyaluronate/carboxymethylcellulose: a comparative study in rats. Am J Surg. 2010; 200:118–123.25. Chao TC, Jeng LB, Lin JD, Chen MF. Reoperative thyroid surgery. World J Surg. 1997; 21:644–647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Hyaluronate-Carboxymethyl Cellulose on Bone Graft Substitute Healing in a Rat Spinal Fusion Model
- The Effect of Hyaluronate-Carboxymethyl Cellulose on Tissue Adhesion after Achilles Tendon Tenorraphy in Rats
- Effect of combined sodium hyaluronate and carboxymethyl cellulose on ocular surface in rat dry eye model
- Efficacy of an Injectable Thermosensitive Gel on Postoperative Adhesion in Rat Model
- A Experimental Study for the Effect of Sodium Carboxymethyl Cellulose on Prevention of Percardial Adhesion