J Korean Soc Radiol.
2013 Jan;68(1):33-41.
Multidetector CT Evaluation of Food Stasis in Remnant Stomach and Body Fat Change after Subtotal Gastrectomy by Laparoscopic versus Open Abdominal Approach
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea. yjsrad97@yuhs.ac
- 2Department of Surgery, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea.
Abstract
- PURPOSE
This study aimed to compare the degree of gastric food stasis and following body fat changes after laparoscopic subtotal gastrectomy (LSTG) versus open subtotal gastrectomy (OSTG).
MATERIALS AND METHODS
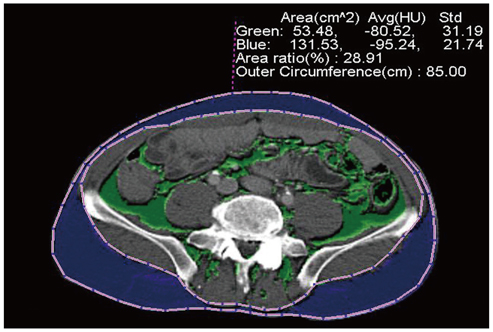
For 284 consecutive gastric cancer patients who underwent subtotal gastrectomy (213 LSTG and 71 OSTG), the one-year follow-up CT images were reviewed retrospectively. The characteristics of gastric stasis was divided into 5 degrees (0, no residue; 1, small secretion; 2, poorly-defined amorphous food; 3, well-delineated measurable food; 4, bezoar-like food). The residual food volume was calculated for the patients with degree 3 or 4 gastric stasis. Postoperative visceral, subcutaneous, and total fat changes were measured on CT and were correlated with the residual food volume.
RESULTS
The LSTG group showed higher degrees of gastric stasis [degree 3 (LSTG, 15.0%; OSTG, 9.9%), degree 4 (LSTG, 6.5%; OSTG, 2.8%)] (p = 0.072). The mean residual food volume of the LSTG group was larger than that of the OSTG group (13779 cc versus 6295 cc) (p = 0.059). Postoperative abdominal fat change was not significantly different between the 2 groups and was not correlated with the residual food volume.
CONCLUSION
LSTG tends to develop gastric stasis more frequently compared with OSTG, but gastric stasis might hardly affect the postoperative body fat status.
MeSH Terms
Figure
Reference
-
1. Jung HJ, Lee JH, Ryu KW, Lee JY, Kim CG, Choi IJ, et al. The influence of reconstruction methods on food retention phenomenon in the remnant stomach after a subtotal gastrectomy. J Surg Oncol. 2008. 98:11–14.2. Watanabe H, Adachi W, Koide N, Yazawa I. Food residue at endoscopy in patients who have previously undergone distal gastrectomy: risk factors and patient preparation. Endoscopy. 2003. 35:397–401.3. Watanabe H, Adachi W, Yazawa K. Endoscopic investigation of food residue in the stomachs of patients having undergone distal gastrectomy. Endosc Forum Dig Dis. 1998. 14:1–6. (in Japanese).4. Diettrich NA, Gau FC. Postgastrectomy phytobezoars--endoscopic diagnosis and treatment. Arch Surg. 1985. 120:432–435.5. Rider JA, Foresti-Lorente RF, Garrido J, Puletti EJ, Rider DL, King AH, et al. Gastric bezoars: treatment and prevention. Am J Gastroenterol. 1984. 79:357–359.6. Nagano H, Ohyama S, Sakamoto Y, Ohta K, Yamaguchi T, Muto T, et al. The endoscopic evaluation of gastritis, gastric remnant residue, and the incidence of secondary cancer after pylorus-preserving and transverse gastrectomies. Gastric Cancer. 2004. 7:54–59.7. Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002. 5:83–89.8. Bowden TA Jr, Hooks VH 3rd, Mansberger AR Jr. The stomach after surgery. An endoscopic perspective. Ann Surg. 1983. 197:637–644.9. Sjöström L, Kvist H, Cederblad A, Tylén U. Determination of total adipose tissue and body fat in women by computed tomography, 40K, and tritium. Am J Physiol. 1986. 250(6 Pt 1):E736–E745.10. Behrns KE, Sarr MG. Diagnosis and management of gastric emptying disorders. Adv Surg. 1994. 27:233–255.11. Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report--a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg. 2010. 251:417–420.12. Yoo CH, Kim HO, Hwang SI, Son BH, Shin JH, Kim H. Short-term outcomes of laparoscopic-assisted distal gastrectomy for gastric cancer during a surgeon's learning curve period. Surg Endosc. 2009. 23:2250–2257.13. Strong VE, Devaud N, Allen PJ, Gonen M, Brennan MF, Coit D. Laparoscopic versus open subtotal gastrectomy for adenocarcinoma: a case-control study. Ann Surg Oncol. 2009. 16:1507–1513.14. Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005. 241:232–237.15. Yakoub D, Athanasiou T, Tekkis P, Hanna GB. Laparoscopic assisted distal gastrectomy for early gastric cancer: is it an alternative to the open approach? Surg Oncol. 2009. 18:322–333.16. Lee JH, Yom CK, Han HS. Comparison of long-term outcomes of laparoscopy-assisted and open distal gastrectomy for early gastric cancer. Surg Endosc. 2009. 23:1759–1763.17. Armbrecht U, Lundell L, Lindstedt G, Stockbruegger RW. Causes of malabsorption after total gastrectomy with Roux-en-Y reconstruction. Acta Chir Scand. 1988. 154:37–41.18. Friess H, Böhm J, Müller MW, Glasbrenner B, Riepl RL, Malfertheiner P, et al. Maldigestion after total gastrectomy is associated with pancreatic insufficiency. Am J Gastroenterol. 1996. 91:341–347.19. Adams JF. The clinical and metabolic consequences of total gastrectomy. I. Morbidity, weight, and nutrition. Scand J Gastroenterol. 1967. 2:137–149.20. Liedman B, Andersson H, Berglund B, Bosaeus I, Hugosson I, Olbe L, et al. Food intake after gastrectomy for gastric carcinoma: the role of a gastric reservoir. Br J Surg. 1996. 83:1138–1143.21. Liedman B, Andersson H, Bosaeus I, Hugosson I, Lundell L. Changes in body composition after gastrectomy: results of a controlled, prospective clinical trial. World J Surg. 1997. 21:416–420. discussion 420-421.22. Kiyama T, Mizutani T, Okuda T, Fujita I, Tokunaga A, Tajiri T, et al. Postoperative changes in body composition after gastrectomy. J Gastrointest Surg. 2005. 9:313–319.23. Yoon DY, Kim HK, Kim JA, Choi CS, Yun EJ, Chang SK, et al. Changes in the abdominal fat distribution after gastrectomy: computed tomography assessment. ANZ J Surg. 2007. 77:121–125.24. Matsuzawa Y. Adipocytokines and metabolic syndrome. Semin Vasc Med. 2005. 5:34–39.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Laparoscopic Approach Also Safe for the Treatment of Remnant Gastric Cancer?
- The Preservation of Left Gastric Atery in Laparoscopy-Assisted Subtotal Gastrectomy with Splenectomy of Stomach Cancer
- Pylorus-Preserving Gastrectomy for Early Gastric Cancer
- The Influence of Operative Approach on Food Retention after Open and Laparoscopy-Assisted Distal Gastrectomy (LADG) for Gastric Cancer
- Ischemic Necrosis of the Gastric Remnant without Splenic Infarction Following Subtotal Gastrectomy