World J Mens Health.
2012 Aug;30(2):146-149.
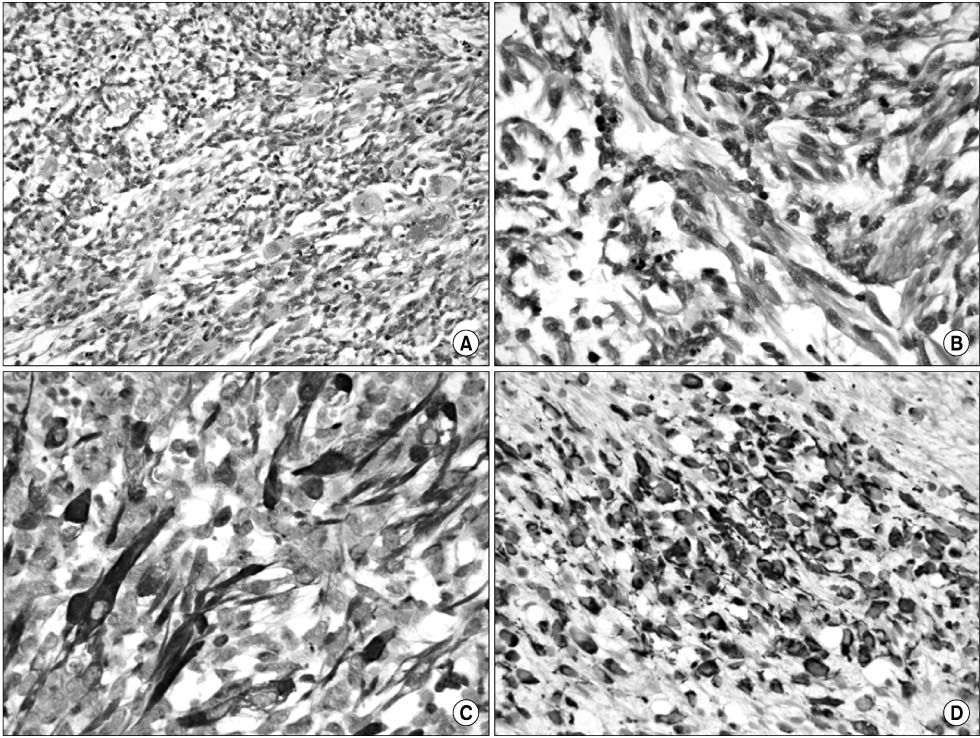
A Case of Pediatric Paratesticular Rhabdomyosarcoma with Epididymitis
- Affiliations
-
- 1Department of Urology, School of Medicine, Jeju National University, Jeju, Korea. mecksd@naver.com
- 2Department of Pathology, School of Medicine, Jeju National University, Jeju, Korea.
Abstract
- Paratesticular rhabdomyosarcoma is a rare malignancy arising from the mesenchymal tissues of the spermatic cord, epididymis, testis, and testicular tunica, and accounts for approximately 7% of all rhabdomyosarcomas. It often occurs in children but is known to have a better prognosis than disease at other urogenital sites. Patients typically present with painless unilateral scrotal swelling like a solid testicular tumor. However, we report an unusual case of delayed diagnosis of paratesticular rhabdomyosarcoma accompanied by epididymitis manifesting an painful scrotal swelling.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim DI, Kim KS. Two cases of pediatric paratesticular rhabdomyosarcoma. Korean J Urol. 2004. 45:1072–1076.2. Qualman S, Lynch J, Bridge J, Parham D, Teot L, Meyer W, et al. Prevalence and clinical impact of anaplasia in childhood rhabdomyosarcoma: a report from the Soft Tissue Sarcoma Committee of the Children's Oncology Group. Cancer. 2008. 113:3242–3247.3. Aquino MR, Gibson DP, Bloom DA. Paratesticular rhabdomyosarcoma with metastatic encasement of the abdominal aorta. Pediatr Radiol. 2011. 41:1061–1064.
Article4. Mak CW, Chou CK, Su CC, Huan SK, Chang JM. Ultrasound diagnosis of paratesticular rhabdomyosarcoma. Br J Radiol. 2004. 77:250–252.
Article5. Akbar SA, Sayyed TA, Jafri SZ, Hasteh F, Neill JS. Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics. 2003. 23:1461–1476.
Article6. Raney RB, Anderson JR, Barr FG, Donaldson SS, Pappo AS, Qualman SJ, et al. Rhabdomyosarcoma and undifferentiated sarcoma in the first two decades of life: a selective review of intergroup rhabdomyosarcoma study group experience and rationale for Intergroup Rhabdomyosarcoma Study V. J Pediatr Hematol Oncol. 2001. 23:215–220.
Article7. Chung JM, Lim YT, Lee SD. Infantile testicular rhabdomyosarcoma. Urology. 2007. 69:1208.
Article