Tuberc Respir Dis.
2014 Oct;77(4):178-183. 10.4046/trd.2014.77.4.178.
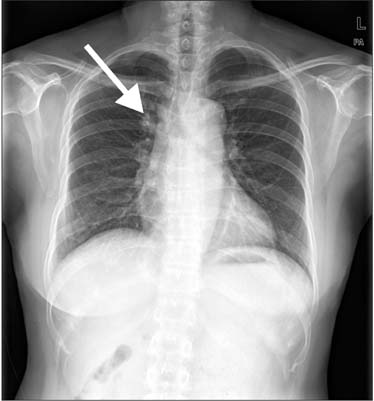
A Case of Delayed Diagnosis of Pulmonary Paragonimiasis due to Improvement after Anti-tuberculosis Therapy
- Affiliations
-
- 1Department of Internal Medicine, Seoul Medical Center, Seoul, Korea. sammy7597@naver.com
- 2Department of Thoracic and Cardiovascular Surgery, Seoul Medical Center, Seoul, Korea.
- 3Department of Radiology, Seoul Medical Center, Seoul, Korea.
- KMID: 2320575
- DOI: http://doi.org/10.4046/trd.2014.77.4.178
Abstract
- Here, we report a case of pulmonary paragonimiasis that was improved with initial anti-tuberculosis (TB) therapy but confused with reactivated pulmonary TB. A 53-year-old Chinese female presented with a persistent productive cough with foul smelling phlegm and blood streaked sputum. Radiologic findings showed subpleural cavitary consolidation in the right upper lobe (RUL). Bronchoscopic and cytological examination showed no remarkable medical feature. She was diagnosed with smear-negative TB, and her radiologic findings improved after receiving a 6-month anti-TB therapy. The chest CT scans, however, obtained at 4 months after completion of anti-TB therapy showed a newly developed subpleural consolidation in the RUL. She refused pathologic confirmation and was re-treated with anti-TB medication. Nevertheless, her chest CT scans revealed newly developed cavitary nodules at 5 months after re-treatment. She underwent thoracoscopic wedge resection; the pathological examination reported that granuloma caused by Paragonimus westermani. Paragonimiasis should also be considered in patients assessed with smear-negative pulmonary TB.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pulmonary Paragonimiasis Misdiagnosed with Pulmonary Tuberculosis
Su Eun Park, Bokyung Song, Jae-Yeon Hwang
Pediatr Infect Vaccine. 2017;24(3):178-182. doi: 10.14776/piv.2017.24.3.178.
Reference
-
1. Yang SP, Huang CT, Cheng CS, Chiang LC. The clinical and roentgenological courses of pulmonary paragonimiasis. Dis Chest. 1959; 36:494–508.2. Singh TS, Mutum SS, Razaque MA. Pulmonary paragonimiasis: clinical features, diagnosis and treatment of 39 cases in Manipur. Trans R Soc Trop Med Hyg. 1986; 80:967–971.3. Kim KU, Lee K, Park HK, Jeong YJ, Yu HS, Lee MK. A pulmonary paragonimiasis case mimicking metastatic pulmonary tumor. Korean J Parasitol. 2011; 49:69–72.4. Siddiqi K, Lambert ML, Walley J. Clinical diagnosis of smear-negative pulmonary tuberculosis in low-income countries: the current evidence. Lancet Infect Dis. 2003; 3:288–296.5. Song JU, Um SW, Koh WJ, Suh GY, Chung MP, Kim H, et al. Pulmonary paragonimiasis mimicking lung cancer in a tertiary referral centre in Korea. Int J Tuberc Lung Dis. 2011; 15:674–679.6. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.7. Kim TS, Han J, Shim SS, Jeon K, Koh WJ, Lee I, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005; 185:616–621.8. Sim YS, Lee JH, Hong SC, Chang JH, Kang SR, Yang HJ, et al. Paragonimus westermani found in the tip of a little finger. Intern Med. 2010; 49:1645–1648.9. Tay NS, Ong KC, Tan SY, Kaw GJ. Tuberculosis mimicry. Eur Respir J. 2005; 26:554–556.10. Moon YR, Lee YD, Park SH, Cho YS, Na DJ, Cho YS, et al. A case of paragonimiasis that was suspicious for a lung malignancy by PET/CT. Tuberc Respir Dis. 2007; 63:521–525.11. Ryu YH, Woo DH, Park JE, Kim HJ, Shin KC, Chung JH, et al. A case of paragonimiasis suspected lung cancer. Yeungnam Univ J Med. 2010; 27:69–73.12. Johnson JR, Falk A, Iber C, Davies S. Paragonimiasis in the United States: a report of nine cases in Hmong immigrants. Chest. 1982; 82:168–171.13. Boland JM, Vaszar LT, Jones JL, Mathison BA, Rovzar MA, Colby TV, et al. Pleuropulmonary infection by Paragonimus westermani in the United States: a rare cause of eosinophilic pneumonia after ingestion of live crabs. Am J Surg Pathol. 2011; 35:707–713.14. Jeon K, Song JU, Um SW, Koh WJ, Suh GY, Chung MP, et al. Bronchoscopic findings of pulmonary paragonimiasis. Tuberc Respir Dis. 2009; 67:512–516.15. Oh IJ, Kim YI, Chi SY, Ban HJ, Kwon YS, Kim KS, et al. Can pleuropulmonary paragonimiasis be cured by only the 1st set of chemotherapy? Treatment outcome and clinical features of recently developed pleuropulmonary paragonimiasis. Intern Med. 2011; 50:1365–1370.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pulmonary Paragonimiasis Mimicking Pulmonary Tuberculosis
- Identification of pulmonary paragonimiasis using Ziehl-Neelsen stain
- A Case of Pulmonary Tuberculosis with Delayed Diagnosis Due to the Temporary Clinical Improvement After Use of Levofloxacin and Amikacin Under the Impression of Community Acquired Pneumonia
- A Case of Paragonimiasis Suspected Lung Cancer
- A Case of Pulmonary Paragonimiasis Mimicking Lung Cancer Diagnosed by EBUS-TBNA