Allergy Asthma Respir Dis.
2020 Jan;8(1):36-39. 10.4168/aard.2020.8.1.36.
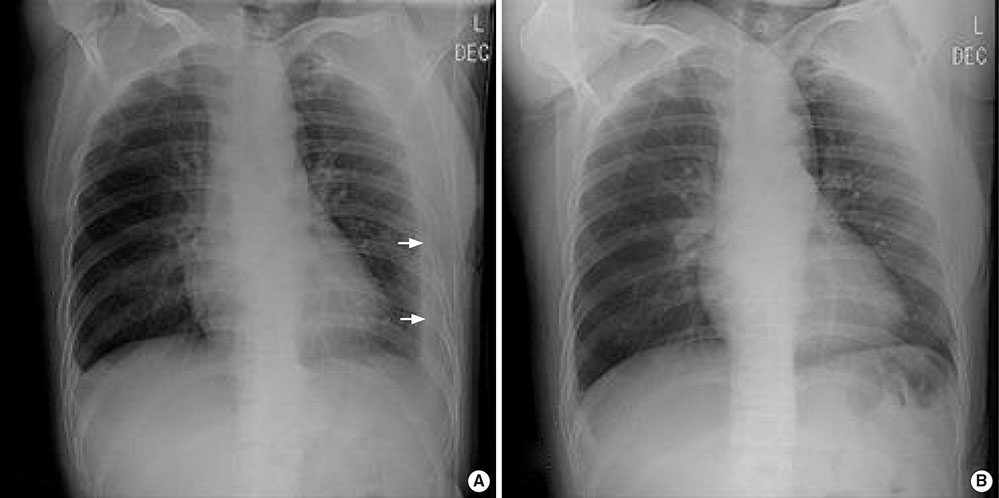
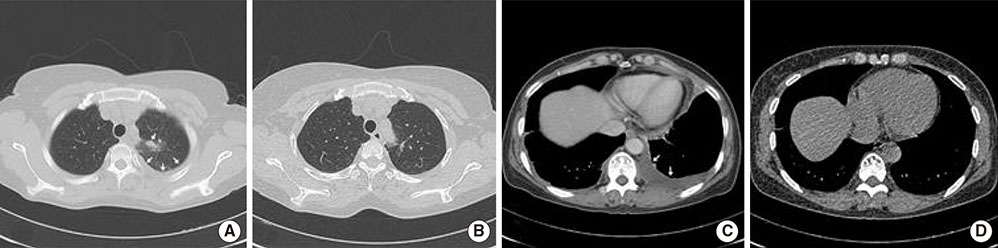
Identification of pulmonary paragonimiasis using Ziehl-Neelsen stain
- Affiliations
-
- 1Department of Medicine, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea. us2001wj@naver.com
- 2Department of Laboratory Medicine, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea.
- 3Department of Radiology, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea.
- KMID: 2469117
- DOI: http://doi.org/10.4168/aard.2020.8.1.36
Abstract
- Pulmonary paragonimiasis and tuberculosis are endemic in Asia, South America, and Africa. However, differential diagnosis among the diseases is difficult because they present with similar clinical symptoms and diagnostic features. Here, we report a case of pulmonary paragonimiasis that was identified using Ziehl-Neelsen stain after initially being assessed for pulmonary tuberculosis. Following anti-Paragonimus chemotherapy, the patient's symptoms, laboratory test results, and lung lesions improved. Thus, the identification of Paragonimus westermani using Ziehl-Neelsen stain can be considered in the diagnosis.
MeSH Terms
Figure
Reference
-
1. Kagawa FT. Pulmonary paragonimiasis. Semin Respir Infect. 1997; 12:149–158.2. Slesak G, Inthalad S, Basy P, Keomanivong D, Phoutsavath O, Khampoui S, et al. Ziehl-Neelsen staining technique can diagnose paragonimiasis. PLoS Negl Trop Dis. 2011; 5:e1048.
Article3. Sim YS, Lee JH, Hong SC, Chang JH, Kang SR, Yang HJ, et al. Paragonimus westermani found in the tip of a little finger. Intern Med. 2010; 49:1645–1648.
Article4. Jeon K, Koh WJ, Kim H, Kwon OJ, Kim TS, Lee KS, et al. Clinical features of recently diagnosed pulmonary paragonimiasis in Korea. Chest. 2005; 128:1423–1430.
Article5. Kim TS, Han J, Shim SS, Jeon K, Koh WJ, Lee I, et al. Pleuropulmonary paragonimiasis: CT findings in 31 patients. AJR Am J Roentgenol. 2005; 185:616–621.
Article6. Sadun EH, Buck AA. Paragonimiasis in South Korea--immunodiagnostic, epidemiologic, clinical, roentgenologic and therapeutic studies. Am J Trop Med Hyg. 1960; 9:562–599.
Article7. Diaz JH. Paragonimiasis acquired in the United States: native and nonnative species. Clin Microbiol Rev. 2013; 26:493–504.
Article8. Im JG, Whang HY, Kim WS, Han MC, Shim YS, Cho SY. Pleuropulmonary paragonimiasis: radiologic findings in 71 patients. AJR Am J Roentgenol. 1992; 159:39–43.
Article9. Hwang KE, Song HY, Jung JW, Oh SJ, Yoon KH, Park DS, et al. Pleural fluid characteristics of pleuropulmonary paragonimiasis masquerading as pleural tuberculosis. Korean J Intern Med. 2015; 30:56–61.
Article10. Im SH, Shin SH, Song MJ, Kim JW, Kim SJ. A case of Paragonimiasis in the abdominal subcutaneous tissue with pleural effusion. Tuberc Respir Dis. 2004; 56:550–554.
Article11. Cho SY, Lee DK, Kang SY, Kim SI. An epidemiological study of human paragonimiasis by means of micro-ELISA. Kisaengchunghak Chapchi. 1983; 21:246–256.
Article12. Kuzucu A. Parasitic diseases of the respiratory tract. Curr Opin Pulm Med. 2006; 12:212–221.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Assessment of Immunohistochemical and Zieh1-Neelsen Stains for Demonstration of Mycobacterium Tuberculosis
- Clinical Usefulness of Polymerase Chain Reaction for the Diagnosis of Pyosalpinx Caused by Tuberculosis
- Acridine orange stain of Mycobacterium leprae
- A Study of the Histopathologic Changes of the Nasal Mucosa in the Patients with Leprosy
- A Prospective Study of Ziehl-Neelsen Stain and Mycobacterial Culture of Pleural Fluid and Closed Pleural Biopsy Specimen in Tuberculous Pleural Effusion