J Korean Ophthalmol Soc.
2016 Jul;57(7):1180-1186. 10.3341/jkos.2016.57.7.1180.
A Case of Posterior Ischemic Optic Neuropathy Accompanied by Carotid Artery Plaque
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. kseeye@hanmail.net
- KMID: 2317584
- DOI: http://doi.org/10.3341/jkos.2016.57.7.1180
Abstract
- PURPOSE
To report a case of posterior ischemic optic neuropathy accompanied by carotid artery plaque in a patient with retrobulbar optic neuritis.
CASE SUMMARY
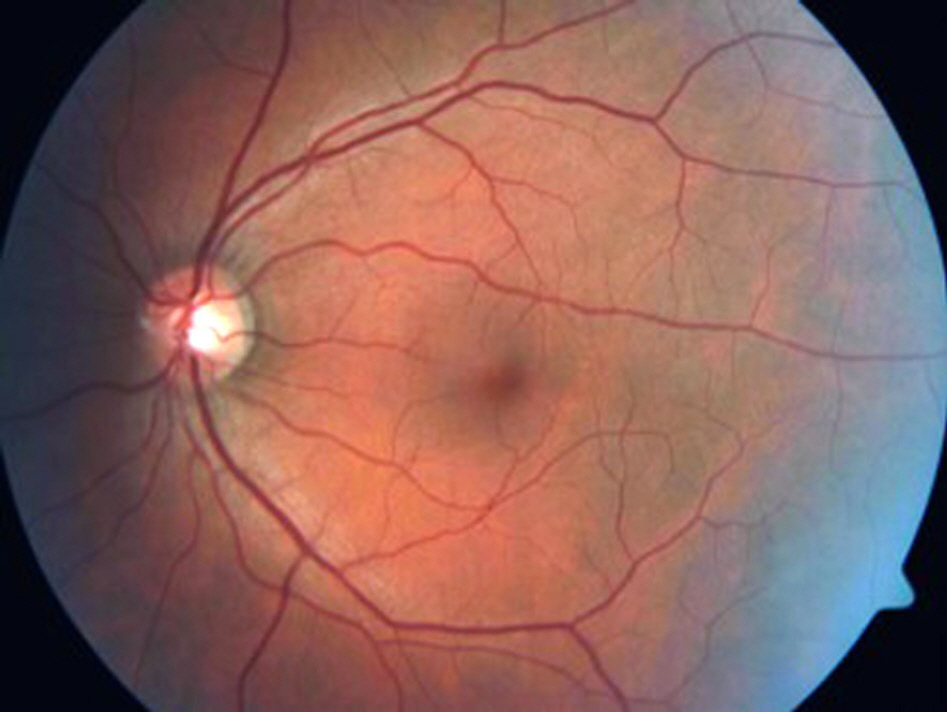
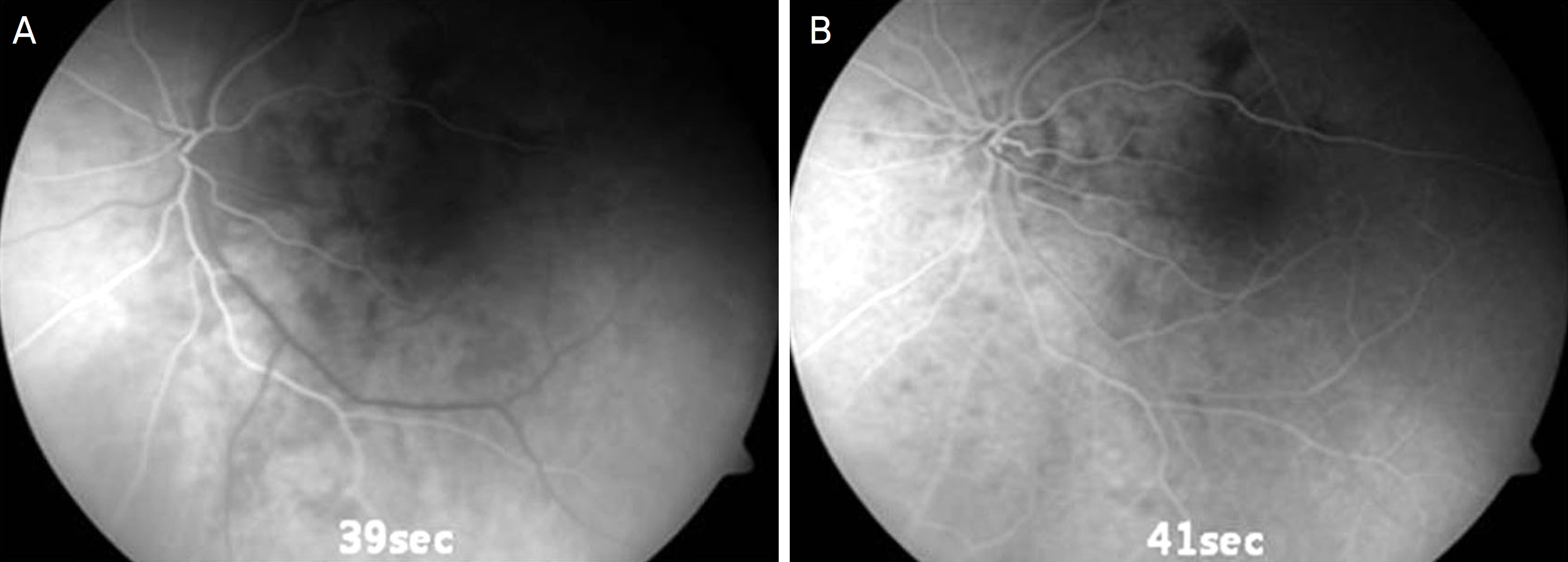
A 48-year-old man visited our clinic complaining of headache, decreasing visual acuity and defect of inferior visual field in his left eye for 3 days. The best corrected visual acuity was 1.0 in the right eye and 0.1 in the left eye. The anterior segment state, intraocular pressure, fundus examination and optical coherence tomography were normal in both eyes. Relative afferent pupillary defect, color vision deficiency and total scotoma were observed in his left eye. The results of the laboratory test and brain magnetic resonance imaging were normal. He was discharged from the hospital after 3 days of systemic steroid treatment on the basis of retrobulbar optic neuritis. A week later, fluorescent angiography and carotid ultrasonography were performed because of his history memory loss and left upper limb weakness before admission. A focal filling defect of the peripapillary area was found on fluorescent angiography. A plaque with a thickness of 1.9 mm and a length of 1.4 cm was found on carotid ultrasonography. After 6 months, the best corrected visual acuity was 0.4 in the left eye and the visual field showed a partially improved defect.
CONCLUSIONS
Fluorescent angiography is recommended for potential posterior ischemic optic neuropathy in patients with retrobulbar optic neuritis, even though it is rare. Carotid ultrasonography is useful in finding atherosclerosis to prevent stroke or cardiovascular disease if ischemic cause is suspected on fluorescent angiography.
Keyword
MeSH Terms
-
Angiography
Atherosclerosis
Brain
Cardiovascular Diseases
Carotid Arteries*
Carotid Stenosis*
Color Vision Defects
Headache
Humans
Intraocular Pressure
Magnetic Resonance Imaging
Memory Disorders
Middle Aged
Optic Neuritis
Optic Neuropathy, Ischemic*
Pupil Disorders
Scotoma
Stroke
Tomography, Optical Coherence
Ultrasonography
Upper Extremity
Visual Acuity
Visual Fields
Figure
Reference
-
References
1. Jung JY, Kim JS. Comparison of optic disc appearance in anterior ischemic optic neuropathy and optic neuritis. J Korean Ophthalmol Soc. 2003; 44:157–61.2. Kim DH, Hwang JM. Risk factors for Korean patients with anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2007; 48:1527–31.
Article3. Park WC, Chang BL. Clinical features of anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2003; 44:144–9.4. Jun BK, Kim DS, Ko MK. Clinical features in anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 1999; 40:3460–7.5. Hayreh SS. Posterior ischaemic optic neuropathy: clinical features, pathogenesis, and management. Eye (Lond). 2004; 18:1188–206.
Article6. Hayreh SS. Ischemic optic neuropathy. Indian J Ophthalmol. 2000; 48:171–94.
Article7. Sadda SR, Nee M, Miller NR, et al. Clinical spectrum of posterior ischemic optic neuropathy. Am J Ophthalmol. 2001; 132:743–50.
Article8. Isayama Y, Takahashi T, Inoue M, Jimura T. Posterior ischemic abdominal neuropathy. III. Clinical diagnosis. Ophthalmologica. 1983; 187:141–7.9. Fazzone HE, Lefton DR, Kupersmith MJ. Optic neuritis: correlation of pain and magnetic resonance imaging. Ophthalmology. 2003; 110:1646–9.10. Lepore FE. The origin of pain in optic neuritis. Determinants of pain in 101 eyes with optic neuritis. Arch Neurol. 1991; 48:748–9.11. Hayreh SS. Posterior ischemic optic neuropathy. Ophthalmologica. 1981; 182:29–41.
Article12. Cullen JF, Por YM. Ischaemic optic neuropathy: the Singapore scene. Singapore Med J. 2007; 48:281–6.13. Schilling H, Mellin KB, Waubke TN. Value of Doppler carotid abdominal sonography in ophthalmologic diagnosis. Fortschr Ophthalmol. 1991; 88:694–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Monocular Superior Altitudinal Field defect due to Supraclinoid Internal Carotid Artery Aneurysm
- A Case of Meningioma Masquerading as Ischemic Optic Neuropathy
- Regrowth of Internal Carotid Artery Aneurysm after Neck Clipping Surgery Presenting with Compressive Optic Neuropathy
- The Etiology of Optic Neuropathy
- A Case of Posterior Ischemic Optic Neuropathy and Abducens Nerve Palsy