J Korean Ophthalmol Soc.
2009 Feb;50(2):324-329. 10.3341/jkos.2009.50.2.324.
A Case of Posterior Ischemic Optic Neuropathy and Abducens Nerve Palsy
- Affiliations
-
- 1Department of Ophthalmology, Kang Dong Sacred Heart Hospital, Seoul, Korea. hyiris@hanmail.net
- KMID: 2212072
- DOI: http://doi.org/10.3341/jkos.2009.50.2.324
Abstract
-
PURPOSE: To report a case of a patient with posterior ischemic optic neuropathy and abducens nerve palsy who responded to steroid therapy.
CASE SUMMARY
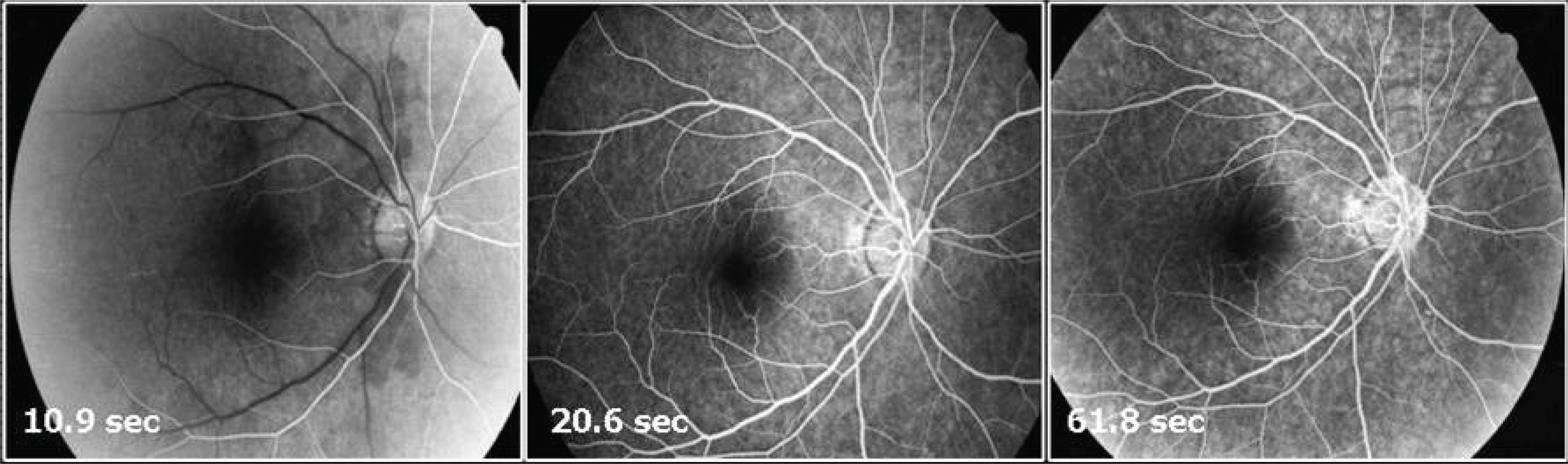
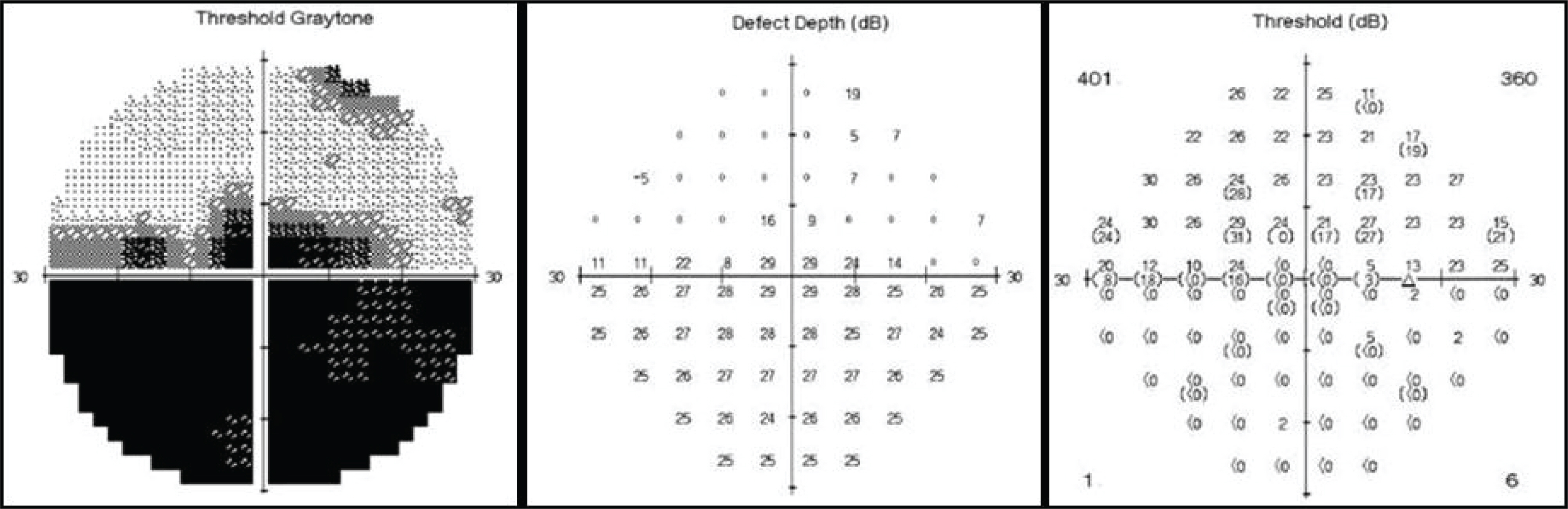
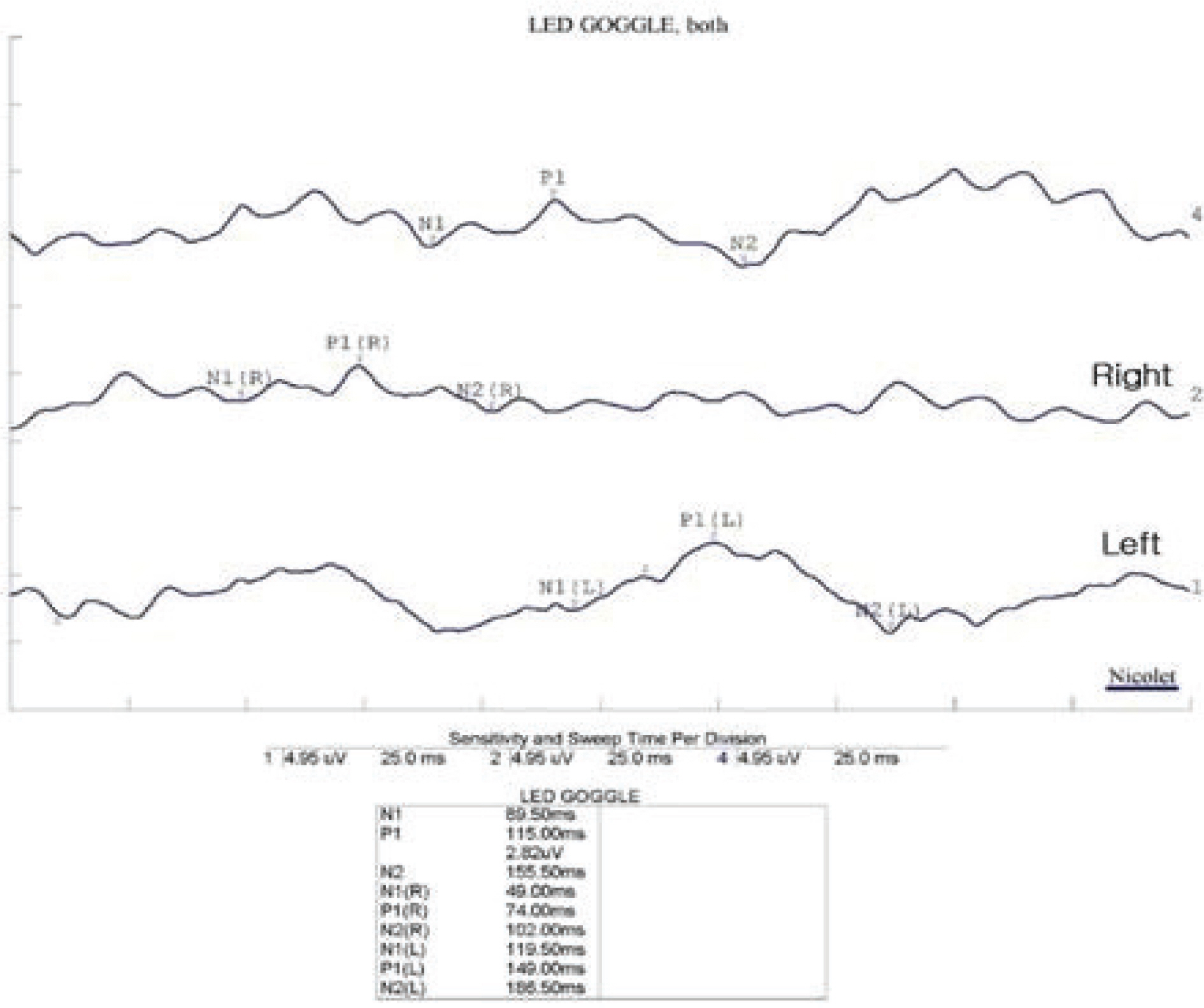
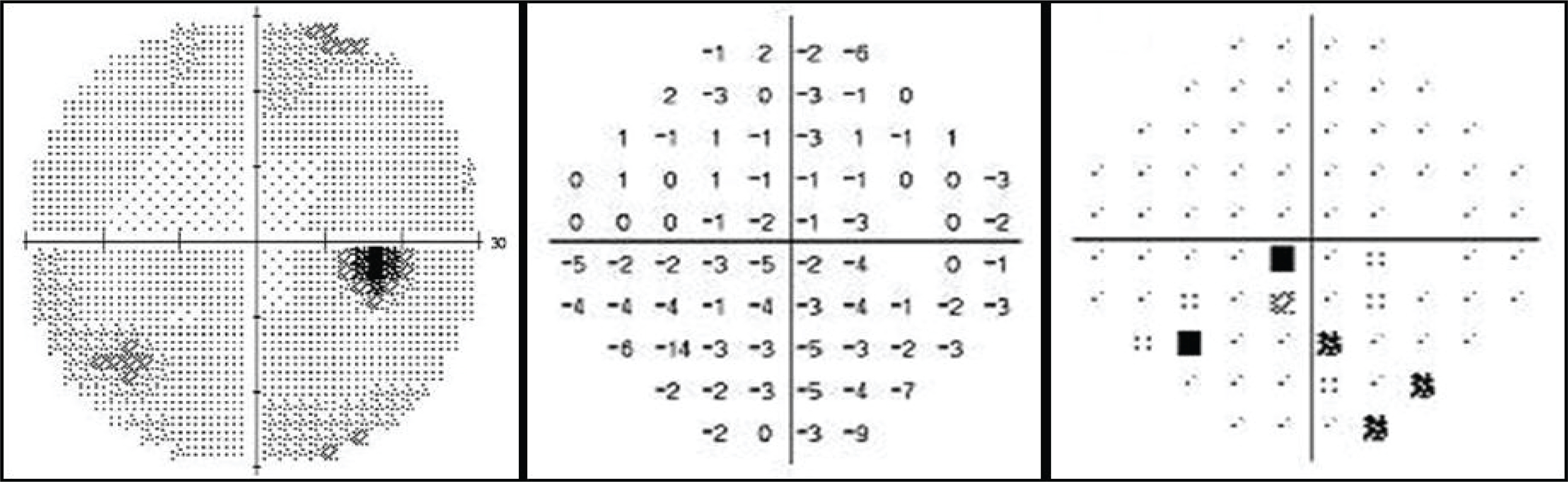
A 47-year-old man visited our clinic with decreasing visual acuity and abduction limitation in his right eye, which suddenly started 4 days earlier. The best corrected visual acuity (BCVA) was 20/250 in the right eye and 20/20 in the left eye. Fundus examination showed normal in both eyes, and relative afferent pupillary defect was positive in the right eye. The visual field test showed a right central scotoma with inferior altitudinal field defect. In addition, the brain magnetic resonance imaging (MRI) was done. Orbit MRI, fluorescein angiography (FAG), and carotid ultrasonography results were normal. Therefore, the patient was diagnosed with non-arteritic posterior ischemic optic neuropathy. The systemic steroid therapy was started and tapered over a period of 5 weeks. At one month after treatment, the BCVA was 20/20 and abduction limitation in the right eye improved.
MeSH Terms
Figure
Reference
-
References
1. Jung JY, Kim JS. Comparison of optic disc appearance in anterior ischemic optic neuropathy and optic neuritis. J Korean Ophthalmol Soc. 2003; 44:157–61.2. Kim DH, Hwang JM. Risk factors for Korean patients with anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2007; 48:1527–31.
Article3. Park WC, Chang BL. Clinical features of anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 2003; 44:144–9.4. Jun BK, Kim DS, Ko MK. Clinical features in anterior ischemic optic neuropathy. J Korean Ophthalmol Soc. 1999; 40:3460–7.5. Hayreh SS. Posterior ischemic optic neuropathy: clinical features, pathogenesis, and management. Eye. 2004; 18:1188–206.6. Hayreh SS. Ischemic optic neuropathy. Indian J Ophthalmol. 2000; 48:171–94.
Article7. Sadda SR, Nee M, Miller NR, et al. Clinical spectrum of posterior ischemic optic neuropathy. Am J Ophthalmol. 2001; 132:743–50.
Article8. Isayama Y, Takahashi T, Inoue M, et al. Posterior ischemic optic neuropathy III. Clinical Diagnosis. Ophthalmologica. 1983; 187:141–7.9. Jeon C, Sa HS, Oh SY. Causes and natural course of the sixth cranial nerve palsy. J Korean Ophthalmol Soc. 2006; 47:1776–80.10. Kim SS, Jin KH, Kim SM. Neuro-opthalmologic evaluation of the third, fourth, and sixth cranial nerve paralysis. J Korean Ophthalmol Soc. 1991; 32:283–8.11. Park KH, Chang BL. The etiology and clinical feature of the third, fourth, and sixth cranial nerve palsy. J Korean Ophthalmol Soc. 1997; 38:1432–6.12. Hayreh SS. Posterior ischemic optic neuropathy. Ophalmologica. 1981; 182:29–41.
Article13. Cullen JF, Por YM. Ischemic optic neuropathy: the Singapore scene. Singapore Med J. 2007; 48:281–6.14. Smith KJ, Mcdonald WI. The pathophysiology of multiple sclerosis: the mechanisms underlying the production of symptoms and the natural history of the disease. Philos Trans R Soc Lond B Biol Sci. 1999; 354:1649–73.
Article15. Milea D, Napolitano M, Dechy H, et al. Complete bilateral horizontal gaze paralysis disclosing multiple sclerosis. J Neurol Neurosurg Psychiatry. 2001; 70:252–5.
Article16. Tan E, Kansu T. Bilateral horizontal gaze palsy in multiple sclerosis. J Clin Neuroophthalmol. 1990; 10:124–6.17. Lee AG. Reversible loss of vision due to posterior ischemic optic neuropathy. Can J Ophthalmol. 1995; 30:327–9.18. Rucker CW. Paralysis of the third, fourth, and sixth cranial nerves. Am J Ophthalmol. 1958; 46:787–94.
Article19. Rucker CW. The causes of paralysis of the third, fourth, and sixth cranial nerves. Am J Ophthalmol. 1966; 61:1293–8.
Article20. Rush JA, Young BR. Paralysis of cranial nerves III, IV, and VI: Cause and prognosis in 1000 cases. Arch Ophthalmol. 1981; 99:76–80.21. Jacobson DM, McCanna TD, Layde PM. Risk factors for ischemic ocular motor nerve palsies. Arch Ophthalmol. 1994; 112:961–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Bilateral Abducens Nerve Palsy after Head Trauma
- A Case of Isolated Unilateral Abducens Nerve Palsy Caused by Clival Metastasis from Rectal Cancer
- Combined Facial and Abducens Nerve Palsy in Pontine Infarction
- Isolated ipsilateral abducens nerve palsy and contralateral homonymous hemianopsia associated with unruptured posterior cerebral artery aneurysm: A rare neurological finding
- The Etiology of Optic Neuropathy