Korean J Urol.
2012 Nov;53(11):755-760.
Clinical Experience with Limited Lymph Node Dissection for Prostate Cancer in Korea: Single Center Comparison of 247 Open and 354 Robot-Assisted Laparoscopic Radical Prostatectomy Series
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cskim@amc.seoul.kr
Abstract
- PURPOSE
There are limited data on the role of limited pelvic lymph node dissection (PLND) in patients with prostate cancer in Korea. The objective of this study was to demonstrate our clinical experience with limited PLND and the difference in its yield between open retropubic radical prostatectomy (RRP) and robot-assisted laparoscopic radical prostatectomy (RALP) for prostate cancer patients in Korea.
MATERIALS AND METHODS
We retrospectively analyzed 601 consecutive patients undergoing radical prostatectomy and bilateral limited PLND by either RRP (n=247) or RALP (n=354) in Asan Medical Center. All patients were divided into three groups according to the D'Amico's risk stratification method. Clinicopathologic data, including the yield of lymph nodes, were thoroughly reviewed and compared among the three risk groups or between the RRP and RALP subjects.
RESULTS
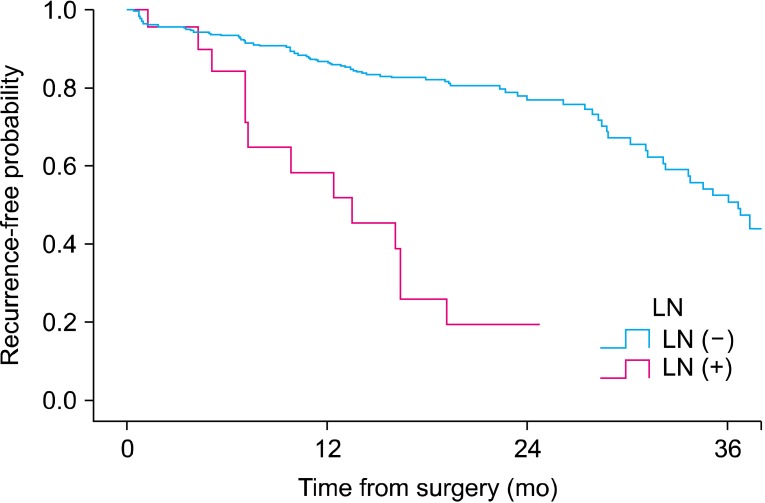
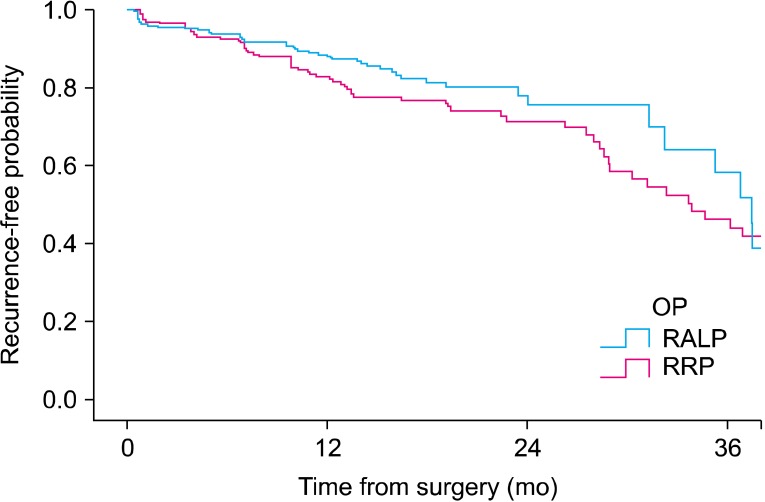
The mean patient age was 64.9 years and the mean preoperative prostate-specific antigen was 9.8 ng/ml. The median number of removed lymph nodes per patient was 5 (range, 0 to 20). The numbers of patients of each risk group were 167, 199, and 238, and the numbers of patients with tumor-positive lymph nodes were 1 (0.6%), 4 (2.0%), and 17 (7.1%) in the low-, intermediate-, and high-risk groups, respectively. In the high-risk group, the lymph node-positive ratio was higher in RRP (14.9%) than in RALP subjects (2.4%).
CONCLUSIONS
We speculate that limited PLND may help in prostate cancer staging in intermediate- and high-risk prostate cancer groups. RRP is a more effective surgical modality for PLND than is RALP, especially in high-risk prostate cancer groups.
MeSH Terms
Figure
Reference
-
1. Jung KW, Park S, Kong HJ, Won YJ, Lee JY, Park EC, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2008. Cancer Res Treat. 2011; 43:1–11. PMID: 21509157.
Article2. Derweesh IH, Kupelian PA, Zippe C, Levin HS, Brainard J, Magi-Galluzzi C, et al. Continuing trends in pathological stage migration in radical prostatectomy specimens. Urol Oncol. 2004; 22:300–306. PMID: 15283887.
Article3. Park SC, Choi HY, Kim CS, Hong SJ, Kim WJ, Lee SE, et al. Predictive variables of the progression to androgen independent prostate cancer after combined androgen blockade. Korean J Urol. 2007; 48:408–415.
Article4. Song C, Ro JY, Lee MS, Hong SJ, Chung BH, Choi HY, et al. Prostate cancer in Korean men exhibits poor differentiation and is adversely related to prognosis after radical prostatectomy. Urology. 2006; 68:820–824. PMID: 17070360.
Article5. Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol. 2011; 59:61–71. PMID: 21056534.
Article6. Briganti A, Blute ML, Eastham JH, Graefen M, Heidenreich A, Karnes JR, et al. Pelvic lymph node dissection in prostate cancer. Eur Urol. 2009; 55:1251–1265. PMID: 19297079.
Article7. Briganti A, Chun FK, Salonia A, Suardi N, Gallina A, Da Pozzo LF, et al. Complications and other surgical outcomes associated with extended pelvic lymphadenectomy in men with localized prostate cancer. Eur Urol. 2006; 50:1006–1013. PMID: 16959399.
Article8. Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982; 128:492–497. PMID: 7120554.
Article9. Tewari A, Takenaka A, Mtui E, Horninger W, Peschel R, Bartsch G, et al. The proximal neurovascular plate and the tri-zonal neural architecture around the prostate gland: importance in the athermal robotic technique of nerve-sparing prostatectomy. BJU Int. 2006; 98:314–323. PMID: 16879671.
Article10. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974. PMID: 9749478.11. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474. PMID: 20180029.
Article12. Burkhard FC, Bader P, Schneider E, Markwalder R, Studer UE. Reliability of preoperative values to determine the need for lymphadenectomy in patients with prostate cancer and meticulous lymph node dissection. Eur Urol. 2002; 42:84–90. PMID: 12160577.
Article13. Heidenreich A, Varga Z, Von Knobloch R. Extended pelvic lymphadenectomy in patients undergoing radical prostatectomy: high incidence of lymph node metastasis. J Urol. 2002; 167:1681–1686. PMID: 11912387.
Article14. Naya Y, Babaian RJ. The predictors of pelvic lymph node metastasis at radical retropubic prostatectomy. J Urol. 2003; 170(6 Pt 1):2306–2310. PMID: 14634402.
Article15. Miki J, Egawa S. The role of lymph node dissection in the management of prostate cancer. Int J Clin Oncol. 2011; 16:195–202. PMID: 21556799.
Article16. Heidenreich A, Pfister D, Thuer D, Brehmer B. Percentage of positive biopsies predicts lymph node involvement in men with low-risk prostate cancer undergoing radical prostatectomy and extended pelvic lymphadenectomy. BJU Int. 2011; 107:220–225. PMID: 20590538.
Article17. Berglund RK, Sadetsky N, DuChane J, Carroll PR, Klein EA. Limited pelvic lymph node dissection at the time of radical prostatectomy does not affect 5-year failure rates for low, intermediate and high risk prostate cancer: results from CaPSURE. J Urol. 2007; 177:526–529. PMID: 17222625.
Article18. Cagiannos I, Karakiewicz P, Eastham JA, Ohori M, Rabbani F, Gerigk C, et al. A preoperative nomogram identifying decreased risk of positive pelvic lymph nodes in patients with prostate cancer. J Urol. 2003; 170:1798–1803. PMID: 14532779.
Article19. Mohler J, Bahnson RR, Boston B, Busby JE, D'Amico A, Eastham JA, et al. NCCN clinical practice guidelines in oncology: prostate cancer. J Natl Compr Canc Netw. 2010; 8:162–200. PMID: 20141676.20. Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC. Natural history of progression after PSA elevation following radical prostatectomy. JAMA. 1999; 281:1591–1597. PMID: 10235151.
Article21. Weckermann D, Goppelt M, Dorn R, Wawroschek F, Harzmann R. Incidence of positive pelvic lymph nodes in patients with prostate cancer, a prostate-specific antigen (PSA) level of < or =10 ng/ml and biopsy Gleason score of < or =6, and their influence on PSA progression-free survival after radical prostatectomy. BJU Int. 2006; 97:1173–1178. PMID: 16686707.22. Schumacher MC, Burkhard FC, Thalmann GN, Fleischmann A, Studer UE. Is pelvic lymph node dissection necessary in patients with a serum PSA < 10 ng/ml undergoing radical prostatectomy for prostate cancer? Eur Urol. 2006; 50:272–279. PMID: 16632187.23. Stone NN, Stock RG, Unger P. Laparoscopic pelvic lymph node dissection for prostate cancer: comparison of the extended and modified techniques. J Urol. 1997; 158:1891–1894. PMID: 9334624.
Article24. Quinn DI, Henshall SM, Brenner PC, Kooner R, Golovsky D, O'Neill GF, et al. Prognostic significance of preoperative factors in localized prostate carcinoma treated with radical prostatectomy: importance of percentage of biopsies that contain tumor and the presence of biopsy perineural invasion. Cancer. 2003; 97:1884–1893. PMID: 12673714.25. Freedland SJ, Aronson WJ, Csathy GS, Kane CJ, Amling CL, Presti JC Jr, et al. Comparison of percentage of total prostate needle biopsy tissue with cancer to percentage of cores with cancer for predicting PSA recurrence after radical prostatectomy: results from the SEARCH database. Urology. 2003; 61:742–747. PMID: 12670558.
Article26. Briganti A, Karakiewicz PI, Chun FK, Gallina A, Salonia A, Zanni G, et al. Percentage of positive biopsy cores can improve the ability to predict lymph node invasion in patients undergoing radical prostatectomy and extended pelvic lymph node dissection. Eur Urol. 2007; 51:1573–1581. PMID: 17293026.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Infected Lymphocele Extending to the Leg after Robot-Assisted Radical Prostatectomy and Pelvic Lymph Node Dissection
- Current technique and results for extended pelvic lymph node dissection during robot-assisted radical prostatectomy
- A Case of Robot-Assisted Laparoscopic Radical Prostatectomy in Primary Small Cell Prostate Cancer
- Robot-Assisted Laparoscopic Radical Prostatectomy
- Robot-Assisted Laparoscopic Radical Cystectomy