Korean J Urol.
2012 Aug;53(8):547-551.
Comparative Evaluation of Periprostatic Nerve Block with and without Intraprostatic Nerve Block in Transrectal Ultrasound-Guided Prostatic Needle Biopsy
- Affiliations
-
- 1Department of Urology, Pandit Bhagwat Dayal Sharma University of Health Sciences, Rohtak, India.
- 2Department of Surgery, Pandit Bhagwat Dayal Sharma University of Health Sciences, Rohtak, India. drashok@fastmail.fm
- 3Department of Radiodiagnosis, Pandit Bhagwat Dayal Sharma University of Health Sciences, Rohtak, India.
Abstract
- PURPOSE
Controversy exists over the pain during prostate biopsy. Periprostatic nerve block is a commonly used anaesthetic technique during transrectal ultrasound (TRUS)-guided prostate biopsy. The recent trend toward increasing the number of cores has become popular. This practice further increases the need for a proper anaesthetic application. We compared the efficacy of periprostatic nerve block with or without intraprostatic nerve block.
MATERIALS AND METHODS
We conducted a prospective double-blinded placebo-controlled study at our institute with 142 consecutive patients. Patients were randomly assigned into 3 groups. Group 1 received periprostatic nerve block with intraprostatic nerve block with 1% lignocaine. Group 2 patients were administered periprostatic nerve block only with 1% lignocaine. Group 3 received no anaesthesia. Patients were asked to grade their level of pain by using an 11-point linear analogue scale at the time of ultrasound probe insertion, at the time of anaesthesia, during biopsy, and 30 minutes after biopsy.
RESULTS
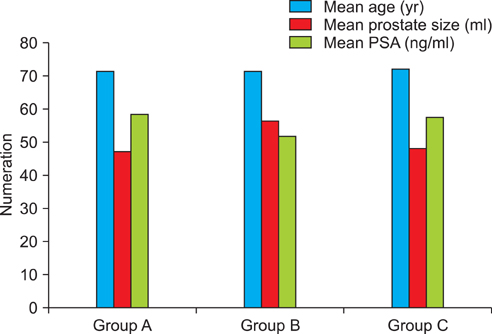
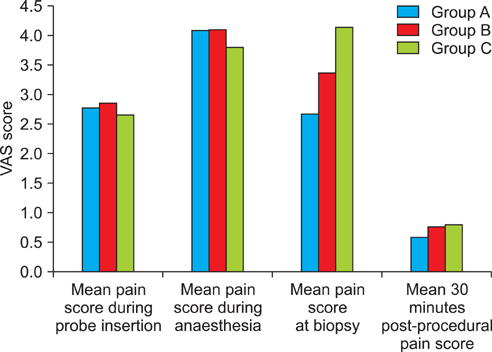
The study groups were comparable in demographic profile, prostate-specific antigen (PSA) level, and prostate size. The mean pain scores at the time of biopsy in groups 1, 2, and 3 were 2.70, 3.39, and 4.16, respectively. Group 1 recorded the minimum mean pain score of 2.70 during prostate biopsy, which was significantly lower than the scores of groups 2 and 3 (p<0.001). There were no significant differences in pain scores among the 3 groups during probe insertion, during anaesthesia, or at 30 minutes after biopsy (p>0.05).
CONCLUSIONS
Periprostatic nerve block with intraprostatic nerve block provides better pain control than does periprostatic nerve block alone in TRUS-guided prostate biopsy.
Keyword
MeSH Terms
Figure
Reference
-
1. Bingqian L, Peihuan L, Yudong W, Jinxing W, Zhiyong W. Intraprostatic local anesthesia with periprostatic nerve block for transrectal ultrasound guided prostate biopsy. J Urol. 2009. 182:479–483.2. Kaver I, Mabjeesh NJ, Matzkin H. Randomized prospective study of periprostatic local anesthesia during transrectal ultrasound-guided prostate biopsy. Urology. 2002. 59:405–408.3. Crundwell MC, Cooke PW, Wallace DM. Patients' tolerance of transrectal ultrasound-guided prostatic biopsy: an audit of 104 cases. BJU Int. 1999. 83:792–795.4. Ochiai A, Babaian RJ. Update on prostate biopsy technique. Curr Opin Urol. 2004. 14:157–162.5. Desgrandchamps F, Meria P, Irani J, Desgrippes A, Teillac P, Le Duc A. The rectal administration of lidocaine gel and tolerance of transrectal ultrasonography-guided biopsy of the prostate: a prospective randomized placebo-controlled study. BJU Int. 1999. 83:1007–1009.6. Hollabaugh RS Jr, Dmochowski RR, Steiner MS. Neuroanatomy of the male rhabdosphincter. Urology. 1997. 49:426–434.7. Conde Redondo C, Alonso FD, Robles SA, Del Valle GN, Castroviejo RF, Delgado MC, et al. TRUS-guided biopsy: comparison of two anesthetic methods. Actas Urol Esp. 2006. 30:134–138.8. Nash PA, Bruce JE, Indudhara R, Shinohara K. Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J Urol. 1996. 155:607–609.9. Soloway MS, Obek C. Periprostatic local anesthesia before ultrasound guided prostate biopsy. J Urol. 2000. 163:172–173.10. Taverna G, Maffezzini M, Benetti A, Seveso M, Giusti G, Graziotti P. A single injection of lidocaine as local anesthesia for ultrasound guided needle biopsy of the prostate. J Urol. 2002. 167:222–223.11. Matlaga BR, Lovato JF, Hall MC. Randomized prospective trial of a novel local anesthetic technique for extensive prostate biopsy. Urology. 2003. 61:972–976.12. Wu CL, Carter HB, Naqibuddin M, Fleisher LA. Effect of local anesthetics on patient recovery after transrectal biopsy. Urology. 2001. 57:925–929.13. Bozlu M, Atici S, Ulusoy E, Canpolat B, Cayan S, Akbay E, et al. Periprostatic lidocaine infiltration and/or synthetic opioid (meperidine or tramadol) administration have no analgesic benefit during prostate biopsy. A prospective randomized double-blind placebo-controlled study comparing different methods. Urol Int. 2004. 72:308–311.14. Mutaguchi K, Shinohara K, Matsubara A, Yasumoto H, Mita K, Usui T. Local anesthesia during 10 core biopsy of the prostate: comparison of 2 methods. J Urol. 2005. 173:742–745.15. Cam K, Sener M, Kayikci A, Akman Y, Erol A. Combined periprostatic and intraprostatic local anesthesia for prostate biopsy: a double-blind, placebo controlled, randomized trial. J Urol. 2008. 180:141–144.16. Lee HY, Lee HJ, Byun SS, Lee SE, Hong SK, Kim SH. Effect of intraprostatic local anesthesia during transrectal ultrasound guided prostate biopsy: comparison of 3 methods in a randomized, double-blind, placebo controlled trial. J Urol. 2007. 178:469–472.17. Moinzadeh A, Mourtzinos A, Triaca V, Hamawy KJ. A randomized double-blind prospective study evaluating patient tolerance of transrectal ultrasound-guided biopsy of the prostate using prebiopsy rofecoxib. Urology. 2003. 62:1054–1057.18. Adiyat KT, Kanagarajah P, PG A, Bhat S. Analgesia for prostate biopsy: efficacy of diclofenac patch versus diclofenac suppository as compared to placebo during prostate biopsy. Int J Nephrol Urol. 2010. 2:239–243.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pain during Transrectal Ultrasound-Guided Prostate Biopsy and the Role of Periprostatic Nerve Block: What Radiologists Should Know
- The Effects of Combination Perianal-Intrarectal Lidocaine-Prilocaine Cream and Periprostatic Nerve Block for Pain Control during Transrectal Ultrasound Guided Biopsy of the Prostate: A Randomized, Controlled Trial
- Comparison of Two Local Anesthestic Methods for Transrectal Ultrasound Guided Prostate Biopsy: Periprostatic Injection of Lidocaine and Rectal Instillation of Lidocaine Gel
- Effect of Periprostatic Nerve Blockade for Transrectal Ultrasound Guided Biopsy of the Prostate
- Effect of Oral Administration of Acetaminophen and Topical Application of EMLA on Pain during Transrectal Ultrasound-Guided Prostate Biopsy