Korean J Urol.
2011 Dec;52(12):835-841.
Early Sequential Changes in Bladder Function after Partial Bladder Outlet Obstruction in Awake Sprague-Dawley Rats: Focus on the Decompensated Bladder
- Affiliations
-
- 1Department of Urology, Inha University College of Medicine by BK 21 Project, Incheon, Korea. lt11@inha.ac.kr
- 2Department of Pharmacology, Inha University College of Medicine by BK 21 Project, Incheon, Korea.
Abstract
- PURPOSE
We investigated bladder function, with special focus on initial functional changes, by objective report of decompensated bladder according to the percentage of residual urine volume to bladder capacity in awake, obstructed rats.
MATERIALS AND METHODS
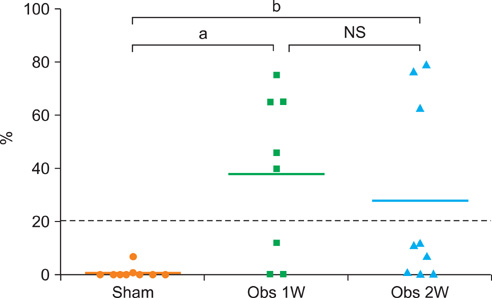
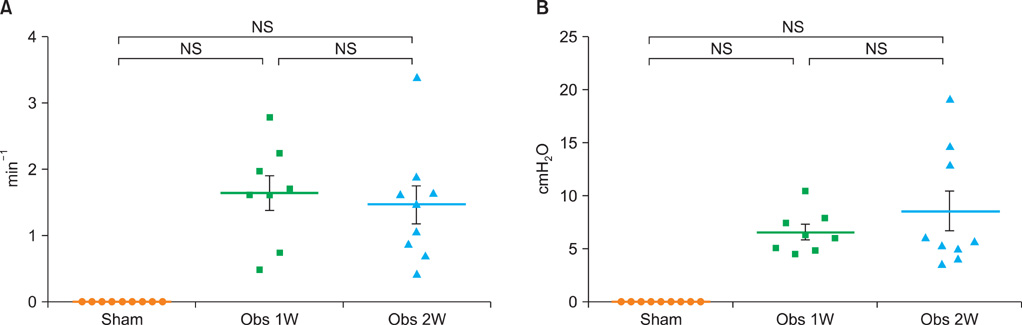
Thirty rats were randomly subjected to sham operations (n=10) or partial bladder outlet obstruction (BOO, n=20). Cystometric investigations were performed without anesthesia 1 or 2 weeks after BOO surgery. To reduce the influence of confounding factors in awake cystometry, we used simultaneous recordings of intravesical and intraabdominal pressures. Decompensated bladder was defined as the bladder with more than 20% of residual volume compared with bladder capacity.
RESULTS
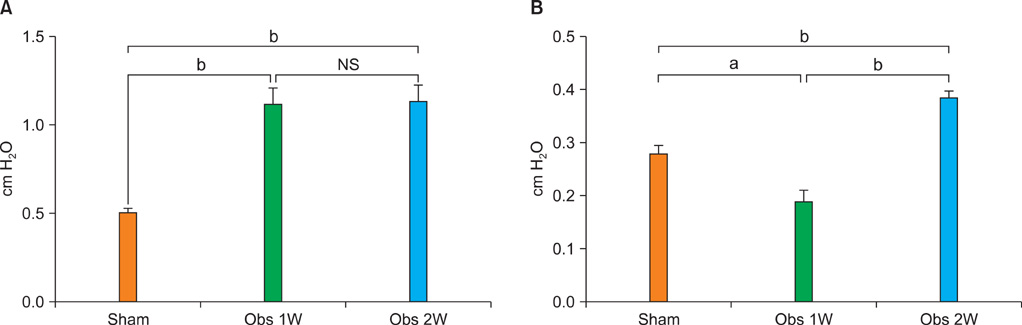
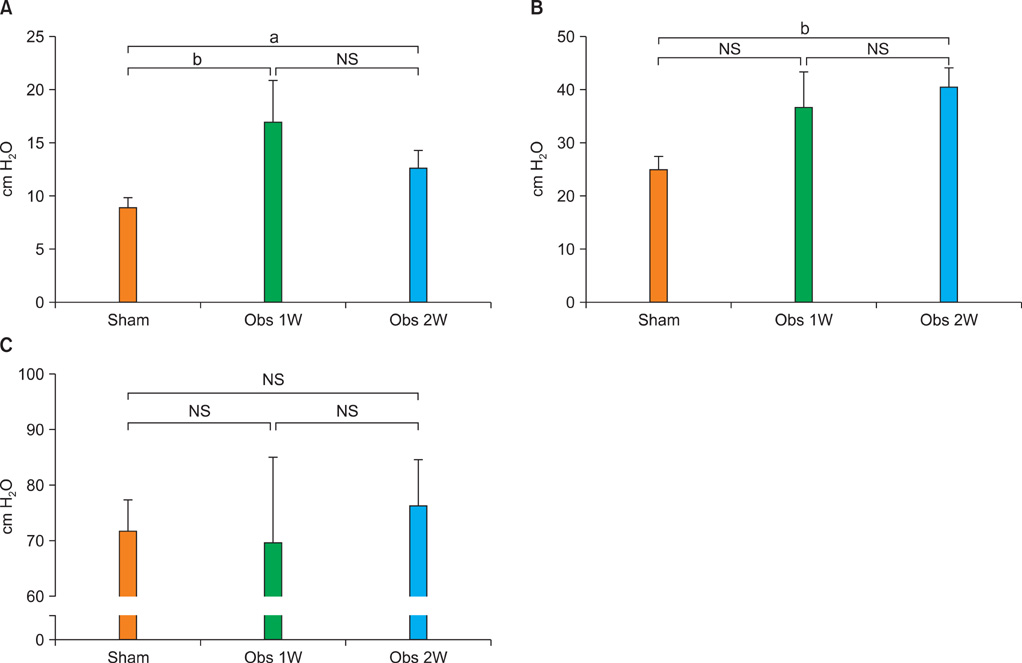
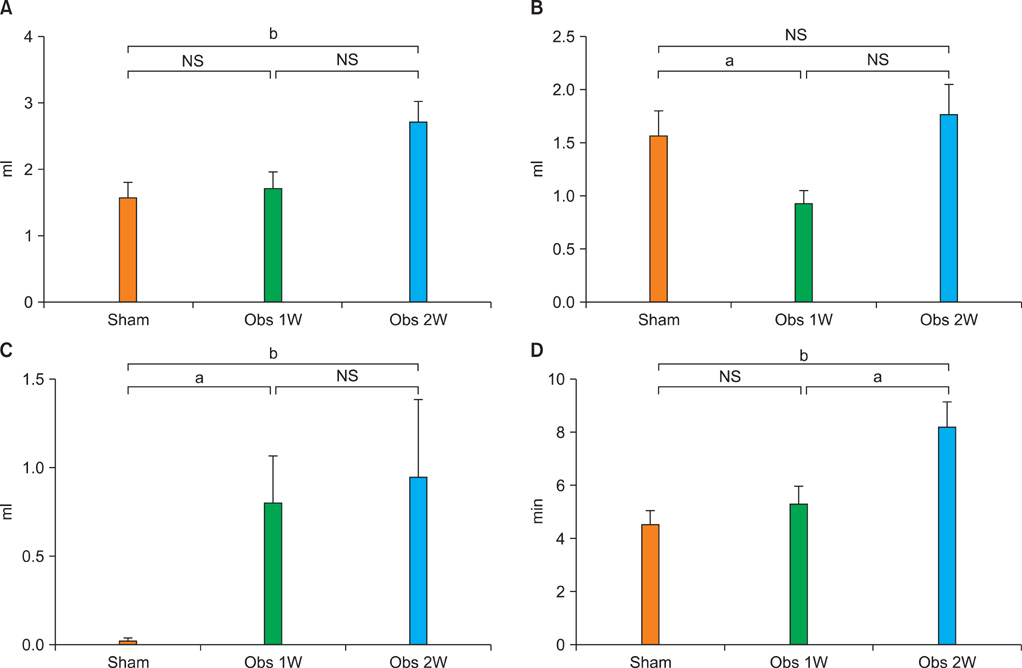
Compared with that in sham animals, basal pressure was elevated in both BOO groups. Threshold pressure was higher in the 2 week BOO (p<0.01) group. Compliance was decreased in the 1 week BOO group (p<0.01) and increased in the 2 week BOO group (p<0.001). Bladder capacity was not increased in the 1 week BOO group, but was increased in the 2 week BOO group (p<0.01). Decompensation was found in 62.5% of the 1 week BOO group and in 33.3% of the 2 week BOO group.
CONCLUSIONS
From the earlier phase, the bladders exhibited serial changes in pressure and volume parameters, and decompensated bladders defined by the percentage of residual volume to bladder capacity could be seen. During the later phase, there was an increasing tendency of compensated bladders, accompanied by the bladders being enlarged and more compliant.
Keyword
MeSH Terms
Figure
Reference
-
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.2. Roberts RO, Jacobsen SJ, Jacobson DJ, Rhodes T, Girman CJ, Lieber MM. Longitudinal changes in peak urinary flow rates in a community based cohort. J Urol. 2000. 163:107–113.3. Chute CG, Panser LA, Girman CJ, Oesterling JE, Guess HA, Jacobsen SJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993. 150:85–89.4. Cuellar DC, Kyprianou N. Future concepts in the medical therapy of benign prostatic hyperplasia. Curr Opin Urol. 2001. 11:27–33.5. Levin RM, Haugaard N, O'Connor L, Buttyan R, Das A, Dixon JS, et al. Obstructive response of human bladder to BPH vs. rabbit bladder response to partial outlet obstruction: a direct comparison. Neurourol Urodyn. 2000. 19:609–629.6. Levin RM, Monson FC, Haugaard N, Buttyan R, Hudson A, Roelofs M, et al. Genetic and cellular characteristics of bladder outlet obstruction. Urol Clin North Am. 1995. 22:263–283.7. O'Connor LT Jr, Vaughan ED Jr, Felsen D. In vivo cystometric evaluation of progressive bladder outlet obstruction in rats. J Urol. 1997. 158:631–635.8. Zderic SA, Rohrmann D, Gong C, Snyder HM, Duckett JW, Wein AJ, et al. The decompensated detrusor II: evidence for loss of sarcoplasmic reticulum function after bladder outlet obstruction in the rabbit. J Urol. 1996. 156:587–592.9. Levin RM, Longhurst PA, Monson FC, Kato K, Wein AJ. Effect of bladder outlet obstruction on the morphology, physiology, and pharmacology of the bladder. Prostate Suppl. 1990. 3:9–26.10. Berggren T, Andersson KE, Lundin S, Uvelius B. Effect and content of arginine vasopressin in normal and obstructed rat urinary bladder: an in vivo and in vitro investigation. J Urol. 1993. 150:1540–1543.11. Malmgren A, Sjögren C, Uvelius B, Mattiasson A, Andersson KE, Andersson PO. Cystometrical evaluation of bladder instability in rats with infravesical outflow obstruction. J Urol. 1987. 137:1291–1294.12. Lee T, Andersson KE, Streng T, Hedlund P. Simultaneous registration of intraabdominal and intravesical pressures during cystometry in conscious rats--effects of bladder outlet obstruction and intravesical PGE2. Neurourol Urodyn. 2008. 27:88–95.13. Jin LH, Andersson KE, Kwon YH, Yoon SM, Lee T. Selection of a control rat for conscious spontaneous hypertensive rats in studies of detrusor overactivity on the basis of measurement of intra-abdominal pressures. Neurourol Urodyn. 2010. 29:1338–1343.14. Levin RM, O'Connor LJ, Leggett RE, Whitbeck C, Chichester P. Focal hypoxia of the obstructed rabbit bladder wall correlates with intermediate decompensation. Neurourol Urodyn. 2003. 22:156–163.15. Schröder A, Chichester P, Kogan BA, Longhurst PA, Lieb J, Das AK, et al. Effect of chronic bladder outlet obstruction on blood flow of the rabbit bladder. J Urol. 2001. 165:640–646.16. Finkbeiner A, Lapides J. Effect of distension on blood flow in dog's urinary bladder. Invest Urol. 1974. 12:210–212.17. Lieb JI, Chichester P, Kogan B, Das AK, Leggett RE, Schröder A, et al. Rabbit urinary bladder blood flow changes during the initial stage of partial outlet obstruction. J Urol. 2000. 164:1390–1397.18. Park SH, Jin LH, Kwon YH, Yoon SM, Ryu JK, Lee T. Application and limitations of awake cystometry in Sprague-Dawley Rats with partial bladder outlet obstruction as a model of overactive bladder or obstruction. Korean J Urol. 2009. 50:486–492.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application and Limitations of Awake Cystometry in Sprague-Dawley Rats with Partial Bladder Outlet Obstruction as a Model of Overactive Bladder or Obstruction
- Effect of Bladder Outlet Obstruction on Blood Flow and Tissue Collagen in Rat Bladder
- The Role of Peripheral and Spinal alpha1-adrenoceptor in Bladder Overactivity Induced by Partial Bladder Outlet Obstruction in Rat
- Ultrastructural Changes of Detrusor Muscle by Partial Obstruction of the Bladder Outlet in the Rat
- Dissimilar Effects of Tolterodine on Detrusor Overactivity in Awake Rats with Chemical Cystitis and Partial Bladder Outlet Obstruction