Korean J Urol.
2009 Sep;50(9):859-864.
Relationships between Relative Proportion of Tissue Components, Urodynamic Parameters, and Low Urinary Tract Symptoms in Patients with Benign Prostatic Hyperplasia
- Affiliations
-
- 1Department of Urology, Eulji Hospital, Eulji University School of Medicine, Seoul, Korea. ytk5202@eulji.ac.kr
- 2Department of Pathology, Eulji Hospital, Eulji University School of Medicine, Seoul, Korea.
Abstract
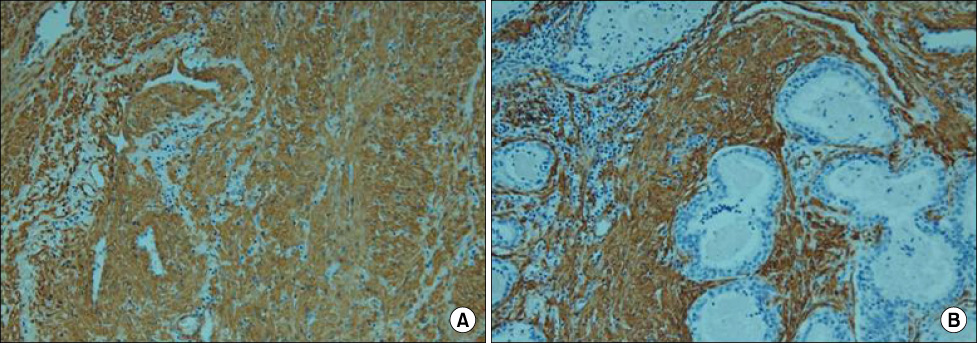
- PURPOSE
This study was designed to investigate the relationship between the histological composition of the prostate, preoperative clinical parameters, and the results of transurethral resection of prostate (TURP). MATERIALS AND METHODS: A total of 61 patients with benign prostatic hyperplasia (BPH) who had undergone TURP were enrolled retrospectively. Slides were surveyed for relative areas (%) of glandular epithelium (GE), stroma (ST), and smooth muscle (SM) in stroma by performing immunohistochemistry, and the mean outcomes were calculated with a computer-assisted image analyzer (x200). RESULTS: Total prostate volume was less than 40 ml in 19 patients (group 1), 40 to 80 ml in 23 patients (group 2), and more than 80 ml in 19 patients (group 3). The percentage of SM was significantly greater in group 1 (29.5+/-4.2%) than in group 3 (23.7+/-3.2%), but GE and ST did not differ significantly. AG number was significantly higher in group 3 than in the other groups but did not correlate with SM. Improvements in International Prostate Symptom Score, which were similar in each group, were positively correlated with SM. CONCLUSIONS: SM in prostate adenoma is increased in men with a small prostate and may play an important role in lower urinary tract symptoms in small BPH
MeSH Terms
Figure
Reference
-
1. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984. 132:474–479.2. Caine M. The present role of alpha-adrenergic blockers in the treatment of benign prostatic hypertrophy. J Urol. 1986. 136:1–4.3. Shapiro E, Becich MJ, Hartanto V, Lepor H. The relative proportion of stromal and epithelial hyperplasia is related to the development of symptomatic benign prostate hyperplasia. J Urol. 1992. 147:1293–1297.4. Byun SS, Jeong H, Jo MK, Lee E. Relative proportions of tissue components in the prostate: Are they related to the development of symptomatic BPH in Korean men? Urology. 2005. 66:593–596.5. McNeal JE. Origin and evolution of benign prostatic enlargement. Invest Urol. 1978. 15:340–345.6. Cadeddu JA, Pearson JD, Lee BR, Landis P, Partin AW, Epstein JI, et al. Relationship between changes in prostate-specific antigen and the percent of prostatic epithelium in men with benign prostatic hyperplasia. Urology. 1995. 45:795–800.7. Bostwick DG, Cooner WH, Denis L, Jones GW, Scardino PT, Murphy GP. The association of benign prostatic hyperplasia and cancer of the prostate. Cancer. 1992. 70(1):Suppl. 291–301.8. Ichiyanagi O, Sasagawa I, Suzuki Y, Ishigooka M, Nakada T. Relation between urethral elasticity and bladder outlet obstruction and histologic composition of the prostate in patients with benign prostatic hyperplasia. Urology. 1999. 53:1149–1153.9. Ishigooka M, Hashimoto T, Suzuki Y, Ichiyanagi O, Sasagawa I, Aoyama N, et al. Functional property, norepinephrine content and morphometric findings in human hyperplastic prostate. Prostate. 1997. 33:183–187.10. Schuster GA, Schuster TG. The relative amount of epithelium, muscle, connective tissue and lumen in prostatic hyperplasia as a function of the mass of tissue resected. J Urol. 1999. 161:1168–1173.11. Ichiyanagi O, Nakada T. Correlations between parameters in pressure-flow analysis and histological compositions in prostate in patients with benign prostatic hyperplasia. Urol Int. 1997. 59:154–160.12. Shapiro E, Hartanto V, Lepor H. Quantifying the smooth muscle content of the prostate using double-immunoenzymatic staining and color assisted image analysis. J Urol. 1992. 147:1167–1170.13. Robert M, Costa P, Bressolle F, Mottet N, Navratil H. Percentage area density of epithelial and mesenchymal components in benign prostatic hyperplasia: comparison of results between single biopsy, multiple biopsies and multiple tissue specimens. Br J Urol. 1995. 75:317–324.14. Ichiyanagi O, Sasagawa I, Ishigooka M, Suzuki Y, Nakada T. Relationship between urodynamic type of obstruction and histological component of the prostate in patients with benign prostatic hyperplasia. Eur Urol. 1999. 36:203–206.15. Ishigooka M, Hashimoto T, Suzuki Y, Ichiyanagi O, Sasagawa I, Aoyama N, et al. Functional property, norepinephrine content and morphometric findings in human hyperplastic prostate. Prostate. 1997. 33:183–187.16. Seo IJ, Seong IG, Han BH. Correlation of histologic types with clinical findings and transrectal ultrasonographic picture in benign prostatic hyperplasia. Korean J Urol. 1996. 37:652–658.17. Ihm JK, Lee YG. Comparison of the finding of transrectal ultrasonography and the result of transrectal resection of prostate according to the histologic types in benign prostatic hyperplasia. Korean J Urol. 2000. 41:1079–1085.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urodynamic Analysis of Men with Lower Urinary Tract Symptoms without Benign Prostatic Hyperplasia
- Current Trend of the Primary Treatment in Lower Urinary Tract Symptom/Benign Prostatic Hyperplasia
- Impact of Bladder Neck Stiffness on Lower Urinary Tract Symptoms in Patient With Benign Prostatic Hyperplasia
- The recovery of the destusor muscle function in acute urinary retention patients due to benign prostatic hyperplasia
- A Clinical Observation on Benign Prostatic Hyperplasia