Korean J Urol.
2009 Dec;50(12):1231-1247.
Nationwide Questionnaire Survey on Practice Patterns for Pediatric Hydronephrosis of Korean Urologists at Secondary or University Hospitals
- Affiliations
-
- 1Department of Urology, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Urology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Urology, College of Medicine, Chonnam National University, Gwangju, Korea.
- 4Department of Urology, College of Medicine, Inha University, Incheon, Korea.
- 5Department of Urology, College of Medicine, Keimyung University, Daegu, Korea.
- 6Department of Urology, College of Medicine, Yonsei University, Seoul, Korea.
- 7Department of Urology, College of Medicine, Pusan National University, Busan, Korea. lsd@pusan.ac.kr
Abstract
- PURPOSE
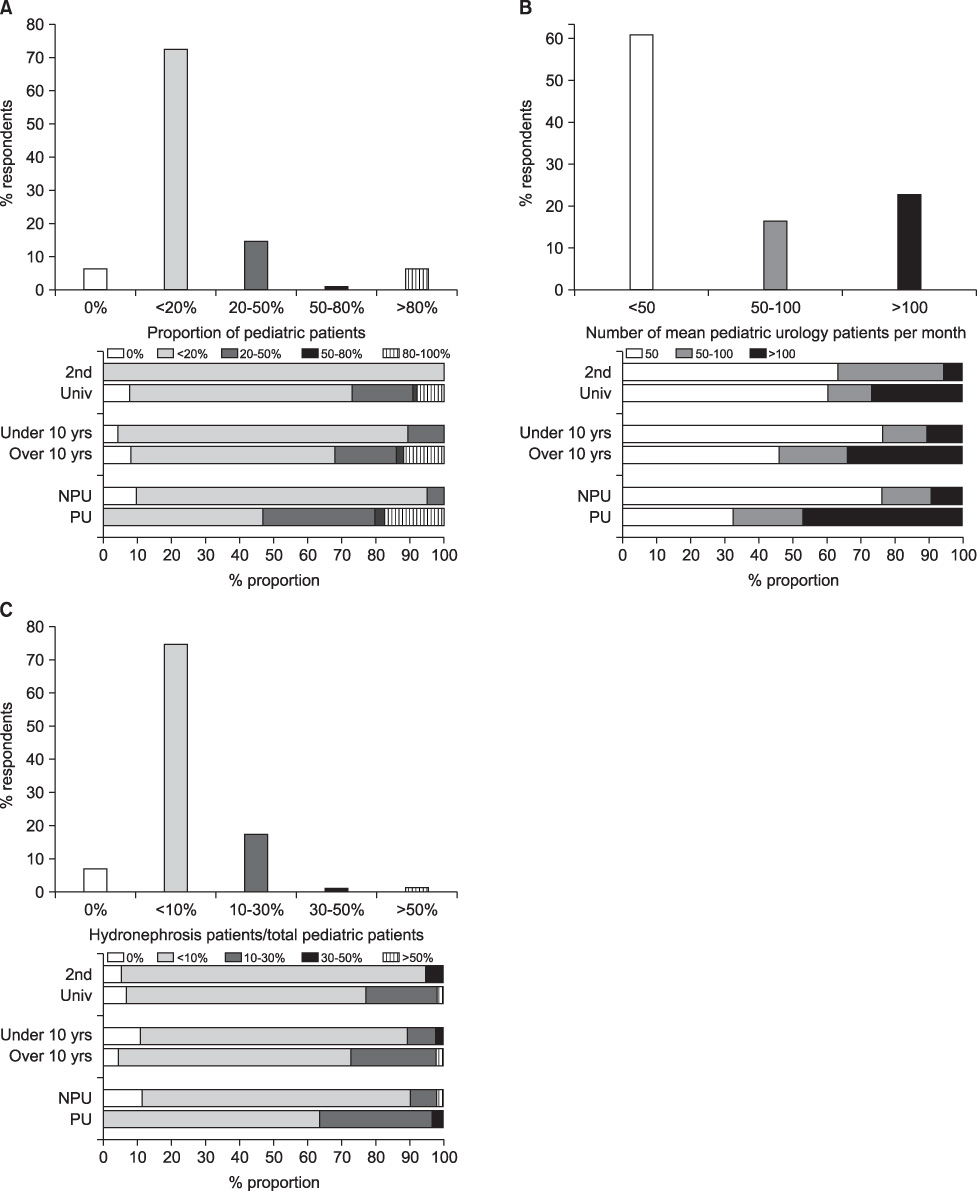
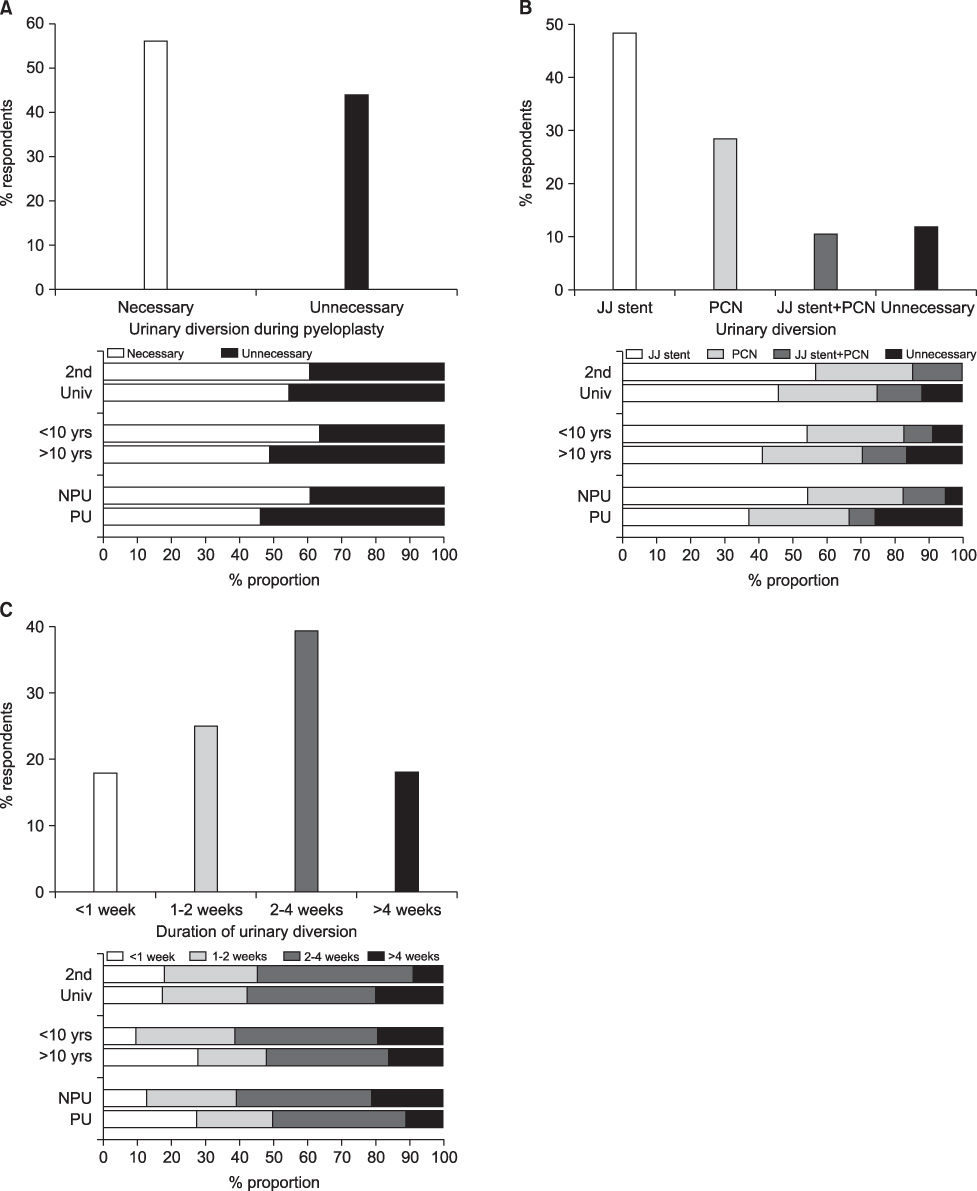
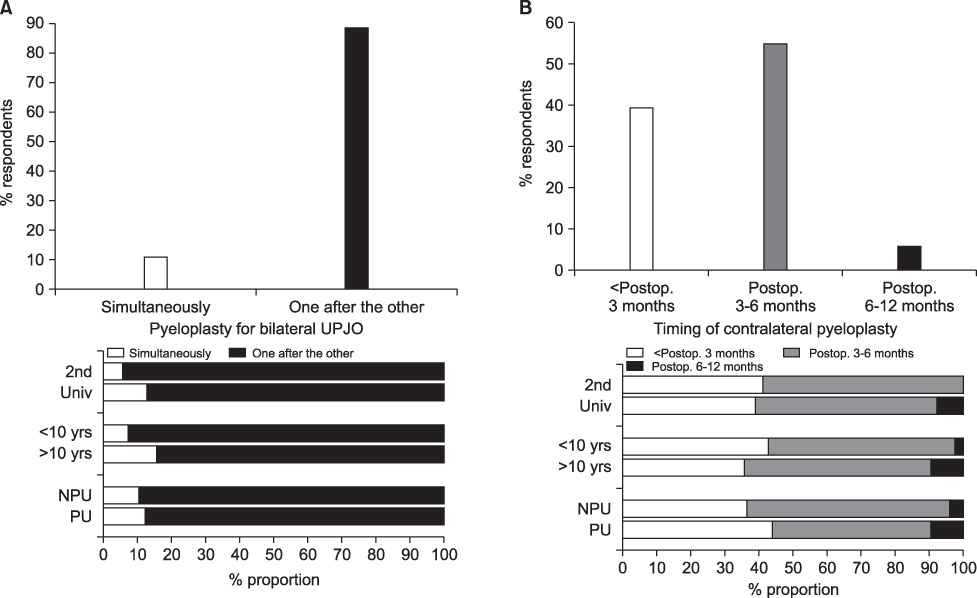
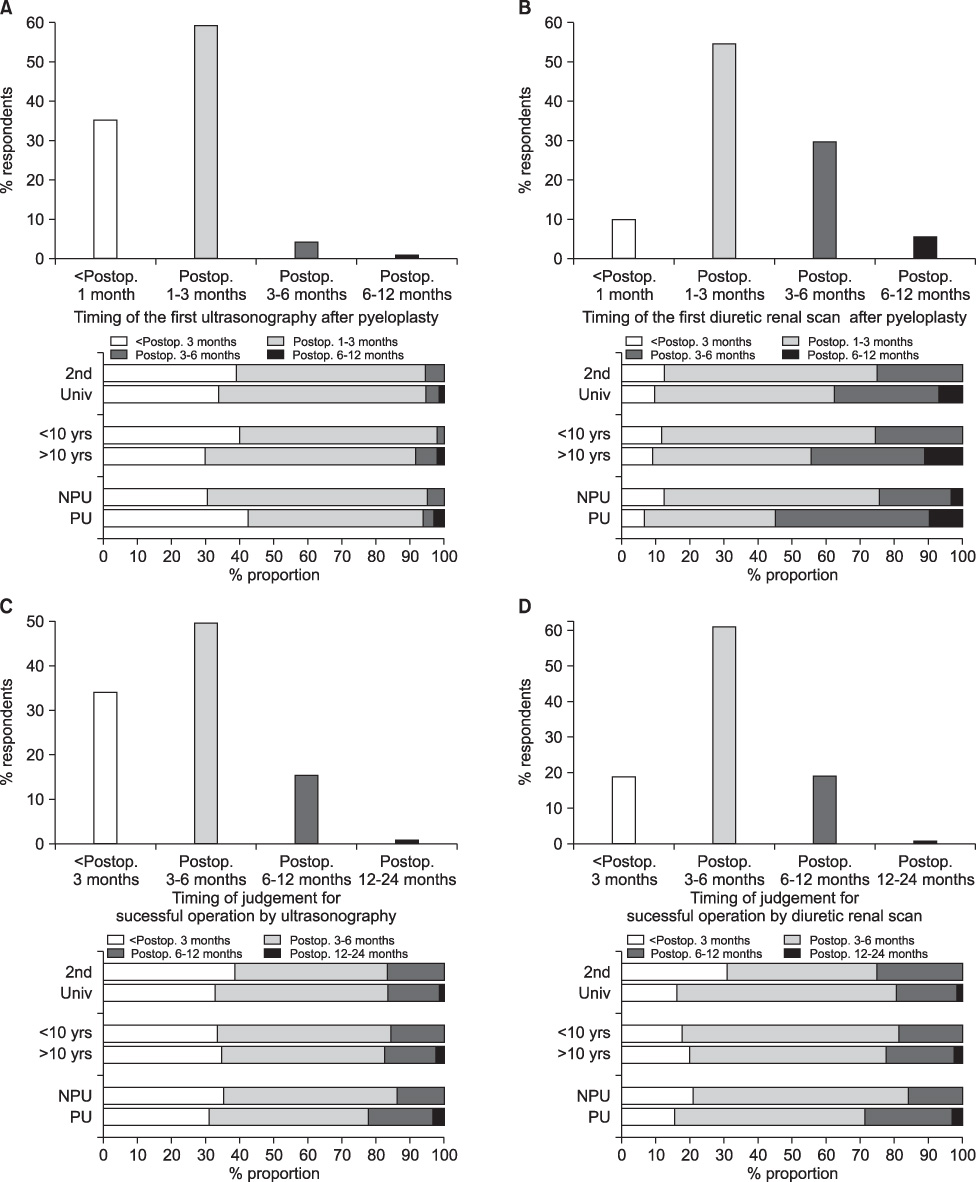
To evaluate practice patterns for pediatric hydronephrosis of Korean urologists practicing at secondary or university hospitals. MATERIALS AND METHODS: The subjects were asked to complete questionnaires sent by postal mail or e-mail that explored practicing diagnostic and therapeutic strategies in the management of pediatric hydronephrosis and ureteropelvic junction obstruction. The questionnaires of those responding were analyzed according to whether the respondent practiced at a secondary or university hospital, how long they had been urologists, and whether they specialized in pediatric urology or other specific field of urology.
RESULTS
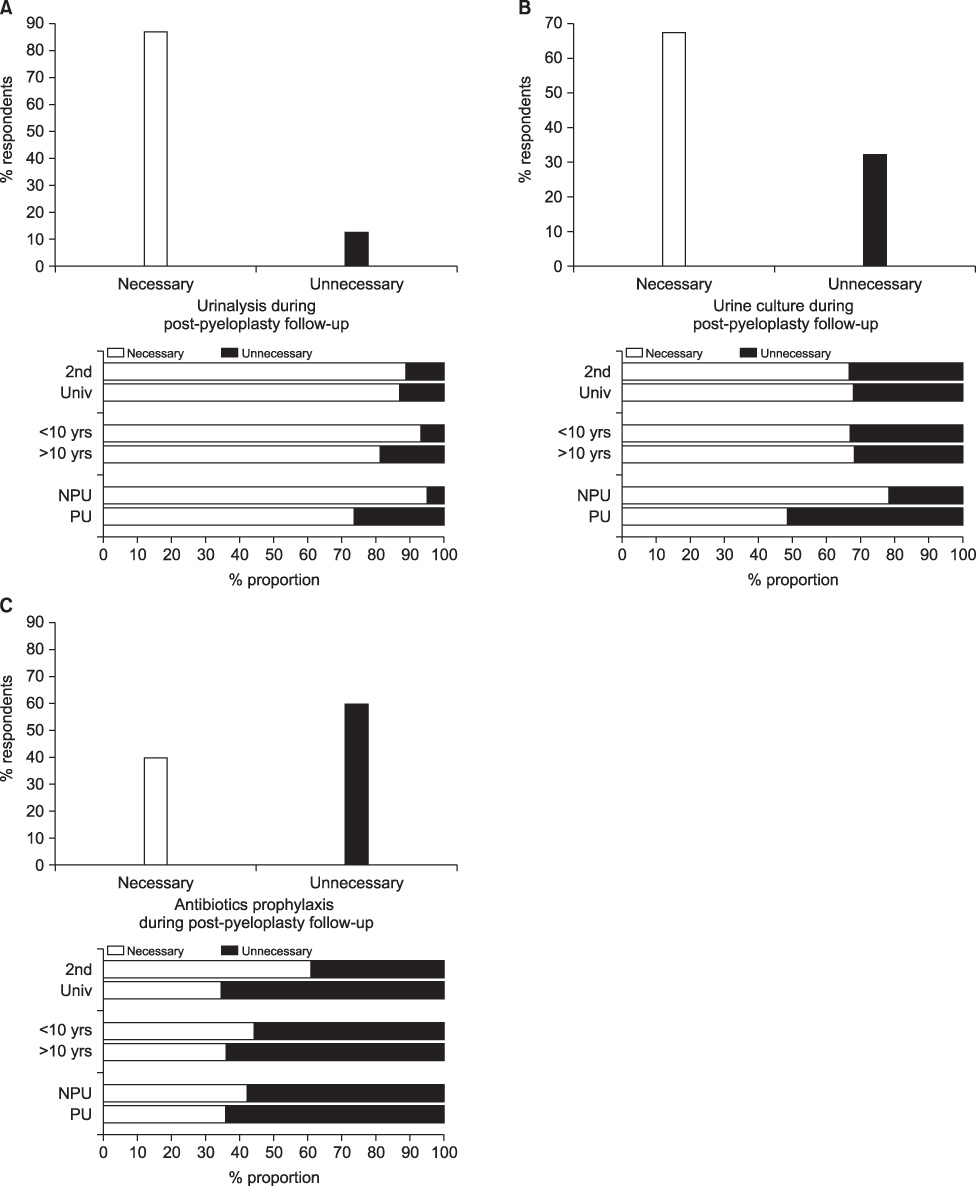
Of the 354 questionnaires sent, 97 were returned (response rate 27.4%). Voiding cystourethrography was not routinely recommended by 95.7% of respondents, and diuretic renal scanning was considered necessary for postnatal evaluation of prenatal hydronephrosis by 78.5%. In addition, 72.2% of these doctors did not routinely recommend antibiotic prophylaxis. Follow-up ultrasonography was recommended at 3 to 6 months (61.1%), and follow-up diuretic renal scanning was recommended at 3 to 6 months (38.6%) or 6 to 12 months (32.7%). The reported length of time it took to deem an operation as a success was 3 to 6 months (49.5% and 60.7%) and within 3 months (34.1% and 19.1%) by ultrasonography and diuretic renal scanning, respectively.
CONCLUSIONS
This survey documented a certain degree of variability among Korean urologists concerning standard practices of the assessment, follow-up, and treatment for pediatric hydronephrosis. Results from this survey might contribute useful data for establishing proper guidelines for the management of pediatric hydronephrosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Roth JA, Diamond DA. Prenatal hydronephrosis. Curr Opin Pediatr. 2001. 13:138–141.2. Lim DJ, Park JY, Kim JH, Paick SH, Oh SJ, Choi H. Clinical characteristics and outcome of hydronephrosis detected by prenatal ultrasonography. J Korean Med Sci. 2003. 18:859–862.3. Choi SM, Jung JH, Hyun JS, Chung KH. Clinical course of prenatally-detected hydronephrosis: focus on ureteropelvic junction obstruction. Korean J Urol. 2008. 49:1125–1130.4. Kang YS, Han SW, Choi SK. The ultrasonographic follow up results and the prognosis of prenatal hydronephrosis. Korean J Urol. 1995. 36:1100–1105.5. Song PH, Cho CK, Park TC. Clinical outcome of prenatal hydronephrosis. Korean J Urol. 2003. 44:556–560.6. Riccabona M. Assessment and management of newborn hydronephrosis. World J Urol. 2004. 22:73–78.7. Harding LJ, Malone PS, Wellesley DG. Antenatal minimal hydronephrosis: Is its follow-up an unnecessary cause of concern? Prenat Diagn. 1999. 19:701–705.8. Dhillon HK. Prenatally diagnosed hydronephrosis: the Great Ormond Street experience. Br J Urol. 1998. 81:Suppl 2. 39–44.9. Riedmiller H, Androulakakis P, Beurton D, Kocvara R, Gerharz E. EAU guidelines on paediatric urology. Eur Urol. 2001. 40:589–599.10. Riccabona M, Avni FE, Blickman JG, Dacher JN, Darge K, Lobo ML, et al. Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol. 2008. 38:138–145.11. Odibo AO, Raab E, Elovitz M, Merrill JD, Macones GA. Prenatal mild pyelectasis: evaluating the thresholds of renal pelvic diameter associated with normal postnatal renal function. J Ultrasound Med. 2004. 23:513–517.12. Fernbach SK, Maizels M, Conway JJ. Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol. 1993. 23:478–480.13. Jaswon MS, Dibble L, Puri S, Davis J, Young J, Dave R, et al. Prospective study of outcome in antenatally diagnosed renal pelvis dilatation. Arch Dis Child Fetal Neonatal Ed. 1999. 80:F135–F138.14. Kim SH, Lee ES, Park JS. The value of voiding cystoureterography on patients with prenatal hydronephrosis: Is it essential? Korean J Urol. 2004. 45:215–218.15. Aksu N, Yavaşcan O, Kangin M, Kara OD, Aydin Y, Erdoğan H, et al. Postnatal management of infants with antenatally detected hydronephrosis. Pediatr Nephrol. 2005. 20:1253–1259.16. Moorthy I, Joshi N, Cook JV, Warren M. Antenatal hydronephrosis: negative predictive value of normal postnatal ultrasound-a 5-year study. Clin Radiol. 2003. 58:964–970.17. Hollowell JG, Altman HG, Snyder HM 3rd, Duckett JW. Coexisting ureteropelvic junction obstruction and vesicoureteral reflux: diagnostic and therapeutic implications. J Urol. 1989. 142:490–493.18. Maizels M, Smith CK, Firlit CF. The management of children with vesicoureteral reflux and ureteropelvic junction obstruction. J Urol. 1984. 131:722–727.19. Canning DA, Nguyen MT. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Evaluation of the pediatric urology patient. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;3189–3216.20. Yerkes EB, Adams MC, Pope JC 4th, Brock JW 3rd. Does every patient with prenatal hydronephrosis need voiding cystourethrography? J Urol. 1999. 162:1218–1220.21. Belarmino JM, Kogan BA. Management of neonatal hydronephrosis. Early Hum Dev. 2006. 82:9–14.22. Ismaili K, Avni FE, Piepsz A, Wissing KM, Cochat P, Aubert D, et al. Current management of infants with fetal renal pelvis dilation: a survey by French-speaking pediatric nephrologists and urologists. Pediatr Nephrol. 2004. 19:966–971.23. Sibley GN, Graham MD, Smith ML, Doyle PT. Improving splintage techniques in pyeloplasty. Br J Urol. 1987. 60:489–491.24. Hendren WH, Radhakrishnan J, Middleton AW Jr. Pediatric pyeloplasty. J Pediatr Surg. 1980. 15:133–144.25. Carr MC, El-ghoneimi A. Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Anomalies and surgery of the ureteropelvic junction in children. Campbell-Walsh urology. 2007. 9th ed. Philadelphia: Saunders;3359–3382.26. Ulman I, Jayanthi VR, Koff SA. The long-term followup of newborns with severe unilateral hydronephrosis initially treated nonoperatively. J Urol. 2000. 164:1101–1105.27. Palmer LS, Maizels M, Cartwright PC, Fernbach SK, Conway JJ. Surgery versus observation for managing obstructive grade 3 to 4 unilateral hydronephrosis: a report from the Society for Fetal Urology. J Urol. 1998. 159:222–228.28. Kim JW, Han SW, Choi SK. The postoperative prognosis of ureteropelvic junction obstruction according to the appearance of the ureter of preoperative retrograde pyelography. Korean J Urol. 2003. 44:550–555.29. Park S, Ji YH, Park YS, Kim KS. Change of hydronephrosis after pyeloplasty in children with unilateral ureteropelvic junction obstruction. Korean J Urol. 2005. 46:586–592.30. Park SJ, Kim YS, Lee HY, Han SW. Appropriate follow-up ultrasonography interval after pyeloplasty in children with ureteropelvic junction obstruction. Korean J Urol. 2008. 49:1018–1023.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comprehension and Practice Patterns of Korean Urologists for Retractile and Gliding Testes
- Comprehension and Practice Patterns Toward Cryptorchidism in Korean Urologists
- Korean Urologist's View of Practice Patterns in Diagnosis and Management of Benign Prostatic Hyperplasia: A Nationwide Survey
- Patterns in the Diagnosis and Management of Benign Prostatic Hyperplasia in a Country that does not have Country-Specific Clinical Practice Guidelines
- Current status of nutritional support for hospitalized children: a nationwide hospital-based survey in South Korea