Ann Rehabil Med.
2016 Apr;40(2):279-287. 10.5535/arm.2016.40.2.279.
Survey of Botulinum Toxin Injections in Anticoagulated Patients: Korean Physiatrists' Preference in Controlling Anticoagulation Profile Prior to Intramuscular Injection
- Affiliations
-
- 1Department of Rehabilitation Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. lafolia@catholic.ac.kr
- 2Department of Rehabilitation Medicine, Pusan National University School of Medicine, Busan, Korea.
- 3Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 4Spasticity Research Program, West Park Healthcare Centre, Toronto, Canada.
- 5Division of Physiatry, Department of Medicine, University of Toronto, Toronto, Canada.
- 6Faculty of Health, York University, Toronto, Canada.
- KMID: 2309927
- DOI: http://doi.org/10.5535/arm.2016.40.2.279
Abstract
OBJECTIVE
To evaluate Korean physiatrists' practice of performing intramuscular botulinum toxin injection in anticoagulated patients and to assess their preference in controlling the bleeding risk before injection.
METHODS
As part of an international collaboration survey study, a questionnaire survey was administered to 100 Korean physiatrists. Physiatrists were asked about their level of experience with botulinum toxin injection, the safe international normalized ratio range in anticoagulated patients undergoing injection, their tendency for injecting into deep muscles, and their experience of bleeding complications.
RESULTS
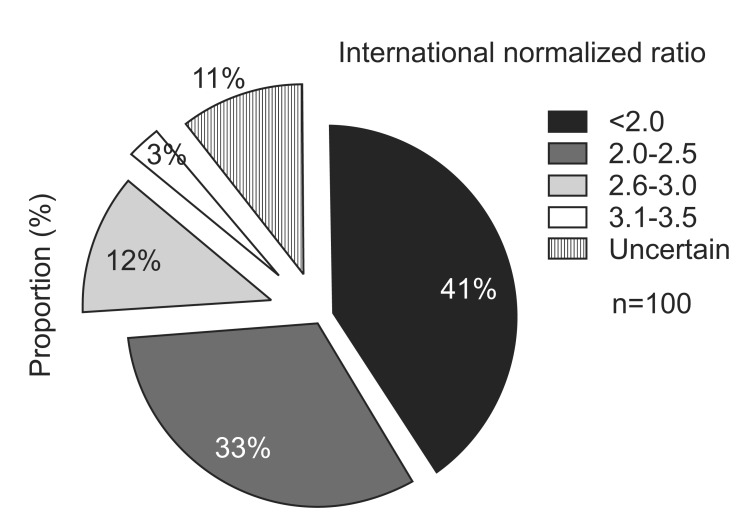
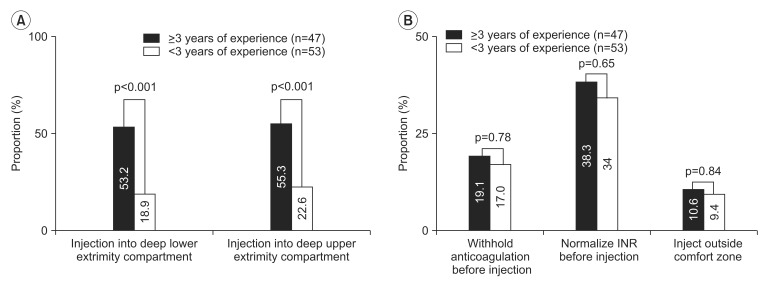
International normalized ratio <2.0 was perceived as an ideal range for performing Botulinum toxin injection by 41% of the respondents. Thirty-six respondents replied that the international normalized ratio should be lowered to sub-therapeutic levels before injection, and 18% of the respondents reported that anticoagulants should be intentionally withheld and discontinued prior to injection. In addition, 20%-30% of the respondents answered that they were uncertain whether they should perform the injection regardless of the international normalized ratio values. About 69% of the respondents replied that they did have any standardized protocols for performing botulinum toxin injection in patients using anticoagulants. Only 1 physiatrist replied that he had encountered a case of compartment syndrome.
CONCLUSION
In accordance with the lack of consensus in performing intramuscular botulinum toxin injection in anticoagulated patients, our survey shows a wide range of practices among many Korean physiatrists; they tend to avoid botulinum toxin injection in anticoagulated patients and are uncertain about how to approach these patients. The results of this study emphasize the need for formulating a proper international consensus on botulinum toxin injection management in anticoagulated patients.
MeSH Terms
Figure
Reference
-
1. Barnes MP, Johnson GR. Upper motor neurone syndrome and spasticity. 2nd ed. New York: Cambridge University Press;2008.2. Wissel J, Manack A, Brainin M. Toward an epidemiology of poststroke spasticity. Neurology. 2013; 80(3 Suppl 2):S13–S19. PMID: 23319481.
Article3. Wissel J, Ward AB, Erztgaard P, Bensmail D, Hecht MJ, Lejeune TM, et al. European consensus table on the use of botulinum toxin type A in adult spasticity. J Rehabil Med. 2009; 41:13–25. PMID: 19197564.
Article4. Olver J, Esquenazi A, Fung VS, Singer BJ, Ward AB. Cerebral Palsy Institute. Botulinum toxin assessment, intervention and aftercare for lower limb disorders of movement and muscle tone in adults: international consensus statement. Eur J Neurol. 2010; 17(Suppl 2):57–73. PMID: 20633179.
Article5. Esquenazi A, Novak I, Sheean G, Singer BJ, Ward AB. International consensus statement for the use of botulinum toxin treatment in adults and children with neurological impairments: introduction. Eur J Neurol. 2010; 17(Suppl 2):1–8. PMID: 20633176.6. Nalysnyk L, Papapetropoulos S, Rotella P, Simeone JC, Alter KE, Esquenazi A. OnabotulinumtoxinA muscle injection patterns in adult spasticity: a systematic literature review. BMC Neurol. 2013; 13:118. PMID: 24011236.
Article7. Boulias C, Ismail F, Trupti S, Phadke CP. Standard of practice in anticoagulated individuals requiring deep compartment botulinum neurotoxin injections for spasticity: a survey. Toxicon. 2015; 93(Suppl):S11–S12.8. Picelli A, Bonetti P, Fontana C, Barausse M, Dambruoso F, Gajofatto F, et al. Accuracy of botulinum toxin type A injection into the gastrocnemius muscle of adults with spastic equinus: manual needle placement and electrical stimulation guidance compared using ultrasonography. J Rehabil Med. 2012; 44:450–452. PMID: 22549655.
Article9. Peck E, Finnoff JT, Smith J, Curtiss H, Muir J, Hollman JH. Accuracy of palpation-guided and ultrasound-guided needle tip placement into the deep and superficial posterior leg compartments. Am J Sports Med. 2011; 39:1968–1974. PMID: 21617254.
Article10. The Stroke Prevention in Atrial Fibrillation Investigators. Bleeding during antithrombotic therapy in patients with atrial fibrillation. Arch Intern Med. 1996; 156:409–416. PMID: 8607726.11. Titolo P, Milani P, Panero B, Ciclamini D, Colzani G, Artiaco S. Acute compartment syndrome of the arm after minor trauma in a patient with optimal range of oral anticoagulant therapy: a case report. Case Rep Orthop. 2014; 2014:980940. PMID: 24516765.
Article12. Zimmerman DC, Kapoor T, Elfond M, Scott P. Spontaneous compartment syndrome of the upper arm in a patient receiving anticoagulation therapy. J Emerg Med. 2013; 44:e53–e56. PMID: 22674040.
Article13. Hylek EM, Skates SJ, Sheehan MA, Singer DE. An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation. N Engl J Med. 1996; 335:540–546. PMID: 8678931.
Article14. Laupacis A, Albers G, Dunn M, Feinberg W. Antithrombotic therapy in atrial fibrillation. Chest. 1992; 102(4 Suppl):426S–433S. PMID: 1395826.
Article15. Boon AJ, Gertken JT, Watson JC, Laughlin RS, Strommen JA, Mauermann ML, et al. Hematoma risk after needle electromyography. Muscle Nerve. 2012; 45:9–12. PMID: 22190299.
Article16. Schrader C, Tacik P, Ebke M, Dressler D. Botulinum toxin therapy in patients with oral anticoagulation: hematoma frequency vs. other side effects [abstract]. Mov Disord. 2012; 27(S1):1099. PMID: 22674458.17. Gertken JT, Patel AT, Boon AJ. Electromyography and anticoagulation. PM R. 2013; 5(5 Suppl):S3–S7. PMID: 23523707.
Article18. Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial. Lancet. 1996; 348:633–638. PMID: 8782752.19. Kearon C, Hirsh J. Management of anticoagulation before and after elective surgery. N Engl J Med. 1997; 336:1506–1511. PMID: 9154771.
Article20. Kim MJ, Park JM, Kim JY, Yoon BW. Etiology and status of preventive therapy of cardioembolic stroke: hospital-based retrospective analysis. J Korean Neurol Assoc. 2005; 23:595–600.21. Petersen P, Boysen G, Godtfredsen J, Andersen ED, Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet. 1989; 1:175–179. PMID: 2563096.22. Brewer MB, Folstein MK, Kerns M, Jesse E. Compartment syndrome of the thigh as a complication of electromyography. Am Surg. 2012; 78:72–73. PMID: 22369800.
Article23. Royal College of Physicians. Spasticity in adults: management using botulinum toxin: national guidelines. London: Royal College of Physician;2009.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction: Survey of Botulinum Toxin Injections in Anticoagulated Patients: Korean Physiatrists' Preference in Controlling Anticoagulation Profile Prior to Intramuscular Injection
- The Effects of Botulinum Toxin (BTXA(R)) Dermal Injections on Facial Wrinkle Lines
- Intradermal Injection of Botulinum Toxin: A Safer Treatment Modality for Forehead Wrinkles
- A CASE REPORT OF TREATMENT OF MASSETERIC HYPERTROPHY WITH BOTULINUM TOXIN
- Botulinum Toxin A Injection into the Subscapularis Muscle to Treat Intractable Hemiplegic Shoulder Pain