J Korean Fract Soc.
2007 Jul;20(3):266-271. 10.12671/jkfs.2007.20.3.266.
Compatibility of Self-setting DBM-CP Composites in Percutaneous Kyphoplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, School of Medicine, Kyung Hee University, Seoul, Korea. ljhos@khmc.or.kr
- KMID: 2296828
- DOI: http://doi.org/10.12671/jkfs.2007.20.3.266
Abstract
- PURPOSE
To analyze the physical properties of demineralized bone matrix (DBM) and self-setting calcium phosphate cement (CPC) composite for its compatibility to percutaneous kyphoplasty.
MATERIALS AND METHODS
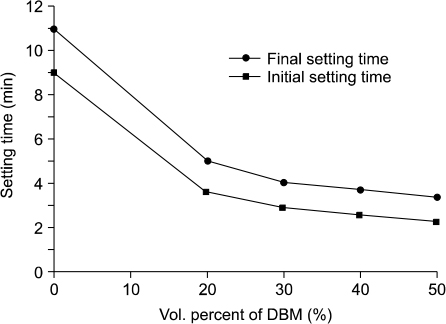
According to tap volume method, DBM was mixed with CPC in variable ratio 0%, 20%, 30%, 40% and 50%. Distilled water was used as a hardening fluid. Its properties, including injectability, mold applicability, setting time and its behavior, maximum temperature, and mechanical strength, were analyzed.
RESULTS
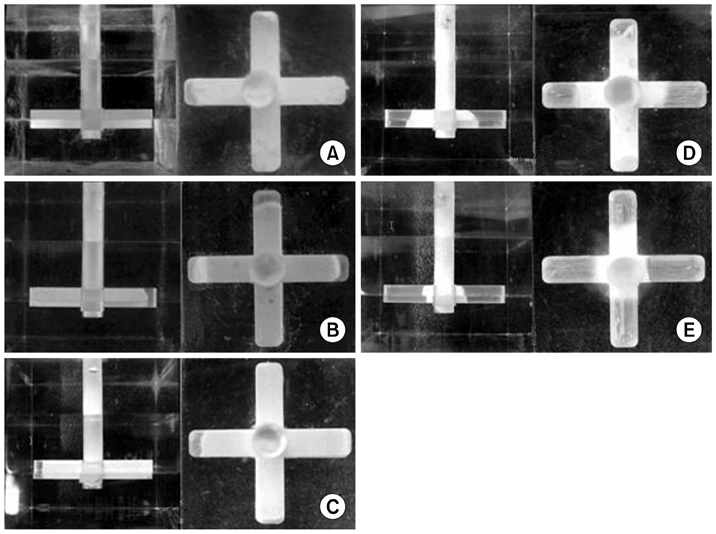
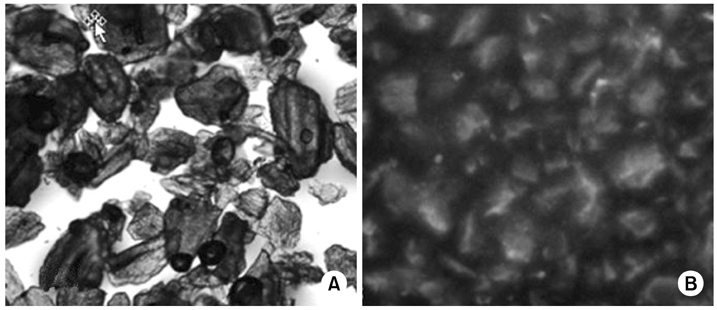
The DBM-CP composites has a good injectability and mold applicability, a maximum temperature of less than 5oC, a initial setting time of 3 to 10 minutes. The outer surface of DBM-CP composites showed their even distribution in optical microscopy. Injectability, mold applicability and compressive strength were in inverse proportion to the amounts of DBM.
CONCLUSION
This study suggests that the DBM-CP composites has a good injectability and mold applicability with a low setting temperature and even distribution of compound. Therefore this composite might be used as a substitute of PMMA in kyphoplasty.
Keyword
MeSH Terms
Figure
Reference
-
1. Allen MJ, Park CK, Yuan PS. Barrier techniques for preventing PMMA induced thermal injury of the spinal cord. In : Proceedings of the 44th Annual Meeting of the Orthopaedic Research Society; Chicago: Rider Dickerson;1998. p. 240.2. Bohner M, Baroud G. Injectability of calcium phosphate pastes. Biomaterials. 2005; 26:1553–1563.
Article3. Brown WB, Chow LC. A new calcium phosphate, watersetting cement. Cements Research Progress. 1986. p. 351–379.4. Chow LC. Development of self-setting calcium phosphate cements. The Centennial Memorial Issue of the Ceramic Society of Japan. 1991; 99:954–964.
Article5. Chow LC, Takagi S, Constantino PD, Friedman CD. Selfsetting calcium phosphate cements. Materials Research Society Symposium Proceedings. 1991; 179:3–24.6. Dahners LE, Jacobs RR. Long bone defects treated with demineralized bone. South Med J. 1985; 78:933–934.
Article7. Freitag TA, Cannon SL. Fracture characteristics of acrylic bone cements. II. Fatigue. J Biomed Mater Res. 1977; 11:609–624.
Article8. Gbureck U, Barralet JE, Spatz K, Grover LM, Thull R. Ionic modification of calcium phosphate cement viscosity. Part I: hypodermic injection and strength improvement of apatite cement. Biomaterials. 2004; 25:2187–2195.
Article9. Gepstein R, Weiss RE, Hallel T. Bridging large defects in bone by demineralized bone matrix in the form of a powder. A radiographic, histological, and radioisotope - uptake study in rats. J Bone Joint Surg Am. 1987; 69:984–992.
Article10. Handal JA, Wallace J, Dossett AB. Autograft vs composite autograft/demineralized bone matrix in spinal fusion. North Am Spine Soc. 1997; 12:333–334.11. Hwang J, Kim JH, Kim JH. Vertebroplasty in the treatment of osteoporotic compression fracture more than 1 year follow up. J Korean Fract Soc. 2004; 17:368–373.
Article12. Johnson JA, Provan JW, Krygier JJ, Chan KH, Miller J. Fatigue of acrylic bone cement - effect of frequency and environment. J Biomed Mater Res. 1989; 23:819–831.13. Khairoun I, Boltong MG, Driessens FC, Planell JA. Some factors controlling the injectability of calcium phosphate bone cements. J Mater Sci Mater Med. 1998; 9:425–428.14. Kim YW, Chang HG, Lee KB, Ji YN, Lee YB, Ku JM. Vertebroplasty for the treatment of painful osteoporotic compression fractures. J Korean Fract Soc. 2004; 17:49–54.
Article15. Konno S, Olmarker K, Byröd G, Nordborg C, Strömgvist B, Rydevik B. The European Spine Society AcroMed Prize 1994. Acute thermal nerve root injury. Eur Spine J. 1994; 3:299–302.16. Lapras C, Mottolese C, Deruty R, Lapras C Jr, Remond J, Duguesnel J. Percutaneous injection of methyl-metacrylate in osteoporosis and severe vertebral osteolysis (Galibert's technic). Ann Chir. 1989; 43:371–376.17. Lowery GL, Maxwell KM, Karasick D. Comparison of autograft and composite grafts of demineralized bone matrix and autologous bone in posterolateral fusions: an interim report. Innov Tech Biol Med. 1995; 16:18.18. Martin G, Boden SD, Morone MA. New formulations of demineralized bone matrix as a more effective graft alternative in experimental posterolateral lumbar spine arthrodesis. Spine. 1999; 24:637–645.
Article19. Mirtchi AA, Lemaitre J, Terao N. Calcium phosphate cements: study of the beta-tricalcium phosphate - monocalcium phosphate system. Biomaterials. 1989; 10:475–480.
Article20. Morone MA, Boden SD. Experimental posterolateral lumbar spinal fusion with a demineralized bone matrix gel. Spine. 1998; 23:159–167.
Article21. Ohura K, Bohner M, Hardouin P, Lemaître J, Pasquier G, Flautre B. Resorption of, and bone formation from, new beta-tricalcium phosphate-monocalcium phosphate cements: an in vivo study. J Biomed Mater Res. 1996; 30:193–200.
Article22. Peters KR, Guiot BH, Martin PA, Fessler RG. Vertebroplasty for osteoporotic compression fractures: current practice and evolving techniques. Neurosurgery. 2002; 51:S96–S103.
Article23. Sassard WR, Eidman DK, Gray PM, et al. Augmenting local bone with Grafton demineralized bone matrix for posterolateral lumbar spine fusion: avoiding second site autologous bone harvest. Orthopedics. 2000; 23:1059–1064.
Article24. Slew S, Chow LC, O'Young A, Tssao NK, Brown W. Evaluation of the biocompatilibity of a new calcium phosphate setting cement. J Dent Res. 1986; 65:195.25. Sugawara A, Chow LC, Takagi S, Chohayeb H. In vitro evaluation of the sealing ability of a calcium phosphate cement when used as a root canal sealer-filler. J Endod. 1990; 16:162–165.
Article26. Tuli SM, Singh AD. The osteoinductive property of decalcified bone matrix. An experimental study. J Bone Joint Surg Br. 1978; 60:116–123.27. Wang JS, Franzen H, Toksvig-Larsen S, Lidgren L. Does vacuum mixing of bone cement affect heat generation? Analysis of four cement brands. J Appl Biomater. 1995; 6:105–108.
Article28. Wu SS, Lachmann E, Nagler W. Current medical, rehabilitation, and surgical management of vertebral compression fractures. J Womens Health (Larchmt). 2003; 12:17–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Results of Percutaneous Kyphoplasty on Vertebral Compression Fractures
- Percutaneous Pediculoplasty and Balloon Kyphoplasty in a Vertebral Metastatic Cancer Patient: A case report
- Asymptomatic Pulmonary Embolus Following Percutaneous Kyphoplasty: A Case Report
- Cauda Equina Syndrome after Percutaneous Balloon Kyphoplasty for Pathologic Compression Fracture
- Benign Cement Leakage after Kyphoplasty: A report of 2 cases