Minimally Invasive Plate Osteosynthesis, MIPO
- Affiliations
-
- 1Department of Orthopedic Surgery, Daegu Fatima Hospital, Korea. fatimaos@unitel.co.kr
- KMID: 2294388
- DOI: http://doi.org/10.12671/jkfs.2007.20.1.99
Abstract
- No abstract available.
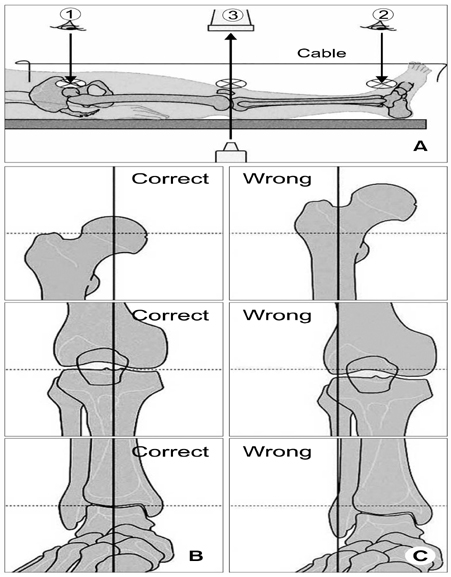
Figure
Cited by 6 articles
-
Minimally Invasive Plate Osteosynthesis for the Upper Extremity Fracture Using a Lumbar Spreader - Surgical Technique -
Gu-Hee Jung, Chyul-Hyun Cho, Jae-Do Kim
J Korean Fract Soc. 2011;24(1):83-86. doi: 10.12671/jkfs.2011.24.1.83.Surgical Techniques for Percutaneous Reduction by Towel Clips and Percutaneous Intramedullary Fixation with Steinmann Pins for Clavicle Shaft Fractures
Ki-Do Hong, Jae-Chun Sim, Sung-Sik Ha, Tae-Ho Kim, Jong-Hyun Kim, Jong-Seong Lee
J Korean Fract Soc. 2012;25(1):31-37. doi: 10.12671/jkfs.2012.25.1.31.The Treatment of Subtrochanteric Fractures with Proximal Femoral Nail Antirotation
Chi Hyoung Pak, Sang Hong Lee, Sang Ho Ha, Gwang Chul Lee, Kyoung Chul Song
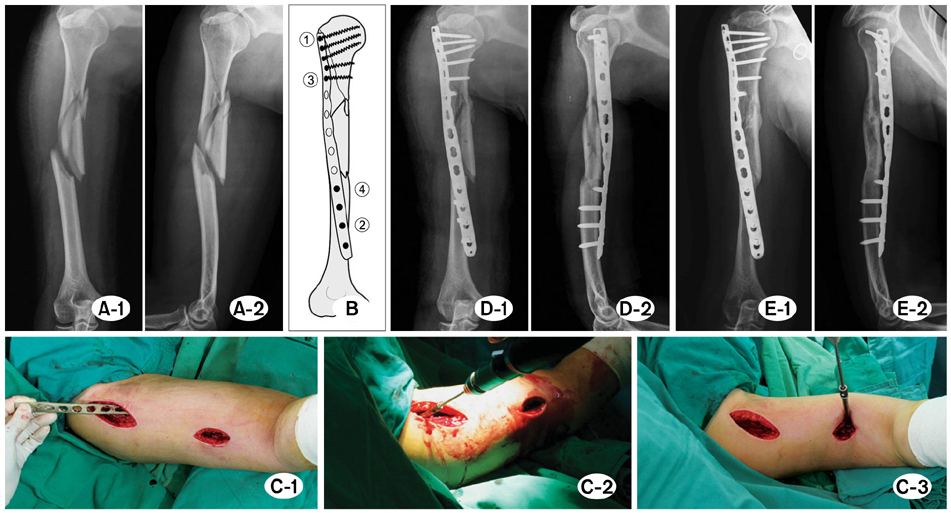
J Korean Fract Soc. 2013;26(4):284-291. doi: 10.12671/jkfs.2013.26.4.284.Minimally Invasive Plate Osteosynthesis Using a Screw Compression Method for Treatment of Humeral Shaft Fractures
Sang-Hun Ko, Jae-Ryong Cha, Chae Chil Lee, Yong Tae Joo, Kyeong Su Eom
Clin Orthop Surg. 2017;9(4):506-513. doi: 10.4055/cios.2017.9.4.506.Axial Malalignment after Minimally Invasive Plate Osteosynthesis in Distal Femur Fractures with Metaphyseal Comminution
Jae-Ho Jang, Gu-Hee Jung, Jae-Do Kim, Cheung-Kue Kim
J Korean Orthop Assoc. 2011;46(4):326-334. doi: 10.4055/jkoa.2011.46.4.326.Anatomical Study of the Pronator Quadratus Muscle and Comparison to Fracture Sites of the Distal Radius
Gu-Hee Jung, Chyul-Hyun Cho, Jae-Do Kim
J Korean Orthop Assoc. 2012;47(1):48-53. doi: 10.4055/jkoa.2012.47.1.48.
Reference
-
1. Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005; 36:530–538.
Article2. Baumgaertel F, Buhl M, Rahn BA. Fracture healing in biological plate osteosynthesis. Injury. 1998; 29:Suppl 3. C3–C6.
Article3. Byun YS, Shin DJ, Chang SA, Kwon DY. Inlay fibular autograft and helical LCP fixation for a segmental comminuted fracture of the osteoporotic proximal humerus: a case report. J Korean Fract Soc. 2006; 19:100–103.
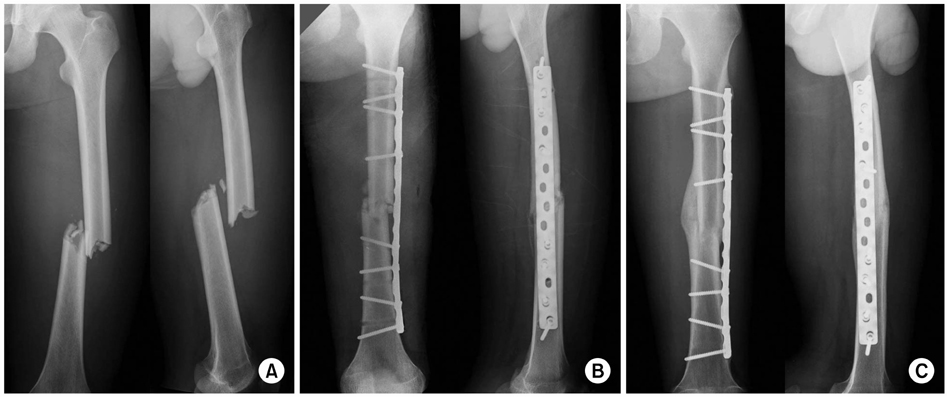
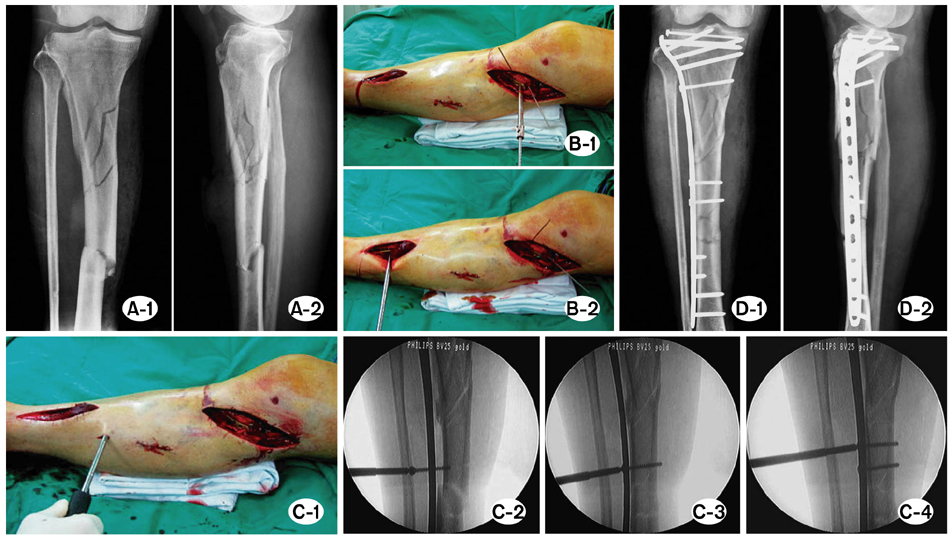
Article4. Chang SA, Ahn HS, Byun YS, Kim JH, Bang HH, Kwon DY. Minimally invasive plate osteosynthesis in unstable fractures of the distal tibia. J Korean Fract Soc. 2005; 18:155–159.
Article5. Cheal EJ, Mansmann KA, DiGioia AM 3rd, Hayes WC, Perren SM. Role of interfragmentary strain in fracture healing: ovine model of a healing osteotomy. J Orthop Res. 1991; 9:131–142.
Article6. Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000; 375:69–77.
Article7. Deangelis JP, Deangelis NA, Anderson R. Anatomy of the superficial peroneal nerve in relation to fixation of tibia fractures with the less invasive stabilization system. J Orthop Trauma. 2004; 18:536–539.
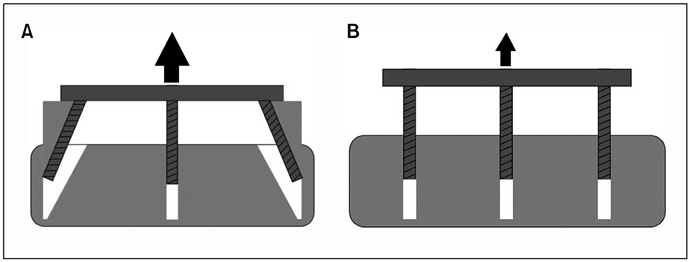
Article8. Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004; 18:488–493.
Article9. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997; 28:Suppl 1. A7–A12.
Article10. Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999; 13:401–406.
Article11. Fernandez Dell'Oca AA. The principle of helical implants. Unusual ideas worth considering. Injury. 2002; 33:Suppl 1. SA1–SA27.12. Frigg R. Development of the locking compression plate. Injury. 2003; 34:Suppl 2. B6–B10.
Article13. Frigg R. Locking compression plate (LCP). An osteosynthesis plate based on the dynamic compression plate and the point contact fixator (PC-Fix). Injury. 2001; 32:Suppl 2. 63–66.
Article14. Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur less invasive stabilization system. Injury. 2001; 32:Suppl 3. SC24–SC31.15. Gautier E, Rahn BA, Perren SM. Vascular remodelling. Injury. 1995; 26:Suppl 2. 11–19.
Article16. Gautier E, Sommer C. Guidelines for the clinical application of the LCP. Injury. 2003; 34:Suppl 2. B63–B76.
Article17. Goodship AE, Kenwright J. The influence of induced micromovement upon the healing of experimental tibial fractures. J Bone Joint Surg Br. 1985; 67:650–655.
Article18. Kim JJ, Kim EG, Choi JW, Park SS. Prediction of rotationally neutral state of the femur by comparing with the shape of contra-lateral lesser trochanter. J Korean Orthop Assoc. 1999; 34:899–903.
Article19. Kinast C, Bolhofner BR, Mast JW, Ganz R. Subtrochanteric fractures of the femur Results of treatment with the 95 degrees condylar blade-plate. Clin Orthop Relat Res. 1989; 238:122–130.20. Krettek C, Miclau T, Grun O, Schandelmaier P, Tscherne H. Intraoperative control of axes, rotation and length in femoral and tibial fractures Technical note. Injury. 1998; 29:C29–C39.
Article21. Krettek C, Miclau T, Stephan C, Tscherne H. Transarticular approach and retrograde plate osteosynthesis for complex distal intraarticular femur fractures. Techniques Orthop. 1999; 14:219–229.
Article22. Krettek C, Rudolf J, Schandelmaier P, Guy P, Konemann B, Tscherne H. Unreamed intramedullary nailing of femoral shaft fractures: operative technique and early clinical experience with the standard locking option. Injury. 1996; 27:233–254.
Article23. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral factures. Injury. 1997; 28:Suppl 1. A20–A30.24. Kubiak EN, Fulkerson E, Strauss E, Egol KA. The evolution of locked plates. J Bone Joint Surg Am. 2006; 88:Suppl 4. 189–200.
Article25. Laurence M, Freeman MA, Swanson SA. Engineering considerations in the internal fixation of fractures of the tibial shaft. J Bone Joint Surg Br. 1969; 51:754–768.
Article26. Mast J, Jacob R, Ganz R. Planning and reduction technique in fracture surgery. 1st ed. Berlin; Heidelberg; New York: Springer-Verlag;1989. p. 11–47. p. 48–129. p. 130–200.27. Miclau T, Martin RE. The evolution of modern plate osteosynthesis. Injury. 1997; 28:Suppl 1. A3–A6.
Article28. Oh CW. Treatment of complex distal tibial fractures. J Korean Fract Soc. 2005; 18:485–490.
Article29. Perren SM. Backgrounds of the technology of internal fixators. Injury. 2003; 34:Suppl 2. B1–B3.
Article30. Perren SM. Evolution and rationale of locked internal fixator technology. Introductory remarks. Injury. 2001; 32:Suppl 2. B3–B9.31. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002; 84:1093–1110.32. Perren SM. The concept of biological plating using the limited contact-dynamic compression plate (LC-DCP). Scientific background, design and application. Injury. 1991; 22:Suppl 1. 1–41.
Article33. Perren SM, Cordey J, Rahn BA, Gautier E, Schneider E. Early temporary porosis of bone induced by internal fixation implants. A reaction to necrosis, not to stress protection. Clin Orthop Relat Res. 1988; 232:139–151.
Article34. Rahn BA, Gallinaro P, Baltensperger A, Perren SM. Primary bone healing. An experimental study in the rabbit. J Bone Joint Surg Am. 1971; 53:783–786.35. Rozbruch RS, Muller U, Gautier E, Ganz R. The evolution of femoral shaft plating technique. Clin Orthop Relat Res. 1998; 354:195–208.
Article36. Ruedi TP, Murphy WM. AO principles of fracture management. 1st ed. Stuttgart; New York: Thieme;2000. p. 7–31. p. 139–155. p. 169–184. p. 195–218. p. 221–230. p. 249–253. p. 290–305.37. Schatzker J. Changes in the AO/ASIF principles and methods. Injury. 1995; 26:51–56.
Article38. Schutz M, Muller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001; 32:Suppl 3. SC48–SC54.
Article39. Stannard JP, Wilson TC, Volgas DA, Alonso JE. Fracture stabilization of proximal tibial fractures with the proximal tibial LISS: early experience in Birmingham, Alabama (USA). Injury. 2003; 34:Suppl 1. A36–A42.
Article40. Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP - how can stability in locked internal fixators be controlled. Injury. 2003; 34:Suppl 2. B11–B19.
Article41. Tepic S, Perren SM. The biomechanics of the PC-Fix internal fixator. Injury. 1995; 26:5–10.
Article42. Tong GO, Bavonratanavech S. AO manual of fracture management. Minimally invasive plate osteosynthesis (MIPO). 1st ed. Stuttgart: Thieme;2007. p. 3–45. p. 66–118. p. 305–325.43. Wagner M. General principles for the clinical use of the LCP. Injury. 2003; 34:Suppl 2. B31–B42.
Article44. Yang KH, Han DY, Park SJ, Yoo HW. Spiral plate fixation for treatment of proximal humerus fracture. J Korean Orthop Assoc. 2000; 35:71–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Percutaneous Plate Stabilization Using a Medial Locking Plate for Proximal Tibial Fractures: Technical Note
- Minimally Invasive Plate Osteosynthesis for the Upper Extremity Fracture Using a Lumbar Spreader: Surgical Technique
- Lateral Plate Fixation of Distal Tibial Metaphyseal Fracture Using Minimally Invasive Plate Osteosynthesis Technique
- Treatment of Distal Femur Fracture with Minimally Invasive Locking Compression Plate Osteosynthesis
- Results of Single Small Incision Minimally Invasive Plate Osteosynthesis in the Treatment of the Distal Radius Fractures