J Korean Fract Soc.
2012 Jan;25(1):13-19. 10.12671/jkfs.2012.25.1.13.
Treatment of Distal Femur Fracture with Minimally Invasive Locking Compression Plate Osteosynthesis
- Affiliations
-
- 1Department of Orthopedic Surgery, Guri Hospital, Hanyang University College of Medicine, Guri, Korea. kcpark@hanyang.ac.kr
- KMID: 1434105
- DOI: http://doi.org/10.12671/jkfs.2012.25.1.13
Abstract
- PURPOSE
To analyze the result of distal femur fracture treatment with minimally invasive plate osteosynthesis (MIPO) using a locking compression plate (LCP).
MATERIALS AND METHODS
From December 2004 to April 2010, 33 patients with distal femur fractures were treated by MIPO with a locking compression plate. The reduction state and bone union time was checked radiologically. The clinical outcome was evaluated by the Schatzker and Lambert criteria.
RESULTS
The mean bone union time was 16.3 weeks (10~22 weeks). There were 3 nonunions, 2 broken plates, 1 superficial infection, 7degrees of valgus angulation in 1 case, and 1.5 cm limb shortening in 1 case. Except for the 3 nonunion cases, according to the Schatzker and Lambert criteria, results were graded as excellent in 11 cases, good in 14 cases, and moderate in 5 cases.
CONCLUSION
The treatment of distal femoral fracture by MIPO with a locking compression plate resulted in good functional and radiological outcomes, but it has problems, such as broken plates and nonunion. Accurate surgical technique and appropriate treatment will be needed according to fracture type.
MeSH Terms
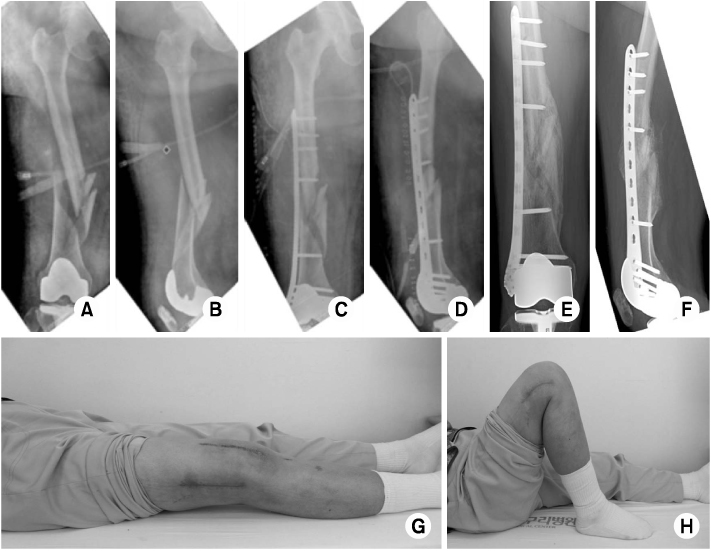
Figure
Cited by 1 articles
-
Minimally Invasive Plate Osteosynthesis with Locking Compression Plate for Distal Femur Fracture
Sung Won Cho, Sang Ho Ha, Gwang Chul Lee, Woong Hee Kim
J Korean Fract Soc. 2013;26(3):205-211. doi: 10.12671/jkfs.2013.26.3.205.
Reference
-
1. Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur: a report of four cases. J Orthop Trauma. 2004. 18:565–570.
Article2. Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 2000. 8:211–216.
Article3. Fankhauser F, Gruber G, Schippinger G, et al. Minimal-invasive treatment of distal femoral fractures with the LISS (Less Invasive Stabilization System): a prospective study of 30 fractures with a follow up of 20 months. Acta Orthop Scand. 2004. 75:56–60.
Article4. Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur Less Invasive Stabilization System (LISS). Injury. 2001. 32:Suppl 3. SC24–SC31.
Article5. Giles JB, DeLee JC, Heckman JD, Keever JE. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am. 1982. 64:864–870.
Article6. Han SB, Choi IC, Lee SH, Suh DH, Cho HJ. Minimal invasive plate osteosynthesis for distal femoral fracture. J Korean Fract Soc. 2006. 19:11–16.7. Henderson CE, Kuhl LL, Fitzpatrick DC, Marsh JL. Locking plates for distal femur fractures: is there a problem with fracture healing? J Orthop Trauma. 2011. 25:Suppl 1. S8–S14.8. Henry SL. Supracondylar femur fractures treated percutaneously. Clin Orthop Relat Res. 2000. (375):51–59.9. Henry SL, Trager S, Green S, Seligson D. Management of supracondylar fractures of the femur with the GSH intramedullary nail: preliminary report. Contemp Orthop. 1991. 22:631–640.10. Kayali C, Agus H, Turgut A. Successful results of minimally invasive surgery for comminuted supracondylar femoral fractures with LISS: comparative study of multiply injured and isolated femoral fractures. J Orthop Sci. 2007. 12:458–465.11. Khan MI. Supracondylar-intercondylar fractures of the femur treated with a supracondylar plate and lag screw. J Bone Joint Surg Am. 1983. 65:135–136.12. Kim SJ, Oh CW, Jeon IH, et al. Minimally invasive plate osteosynthesis for distal femoral fractures. J Korean Soc Fract. 2003. 16:474–481.
Article13. Koval KJ, Hoehl JJ, Kummer FJ, Simon JA. Distal femoral fixation: a biomechanical comparison of the standard condylar buttress plate, a locked buttress plate, and the 95-degree blade plate. J Orthop Trauma. 1997. 11:521–524.
Article14. Kregor PJ, Stannard JA, Zlowodzki M, Cole PA, Alonso J. Distal femoral fracture fixation utilizing the Less Invasive Stabilization System (L.I.S.S.): the technique and early results. Injury. 2001. 32:Suppl 3. SC32–SC47.15. Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004. 18:509–520.16. Krettek C, Schandelmaier P, Miclau T, Bertram R, Holmes W, Tscherne H. Transarticular joint reconstruction and indirect plate osteosynthesis for complex distal supracondylar femoral fractures. Injury. 1997. 28:Suppl 1. A31–A41.
Article17. Lucas SE, Seligson D, Henry SL. Intramedullary supracondylar nailing of femoral fractures. A preliminary report of the GSH supracondylar nail. Clin Orthop Relat Res. 1993. (296):200–206.
Article18. Markmiller M, Konrad G, Südkamp N. Femur-LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications? Clin Orthop Relat Res. 2004. (426):252–257.
Article19. Neer CS 2nd, Grantham SA, Shelton ML. Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am. 1967. 49:591–613.
Article20. Ostrum RF, Geel C. Indirect reduction and internal fixation of supracondylar femur fractures without bone graft. J Orthop Trauma. 1995. 9:278–284.
Article21. Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002. 84:1093–1110.
Article22. Schatzker J, Home G, Waddell J. The Toronto experience with the supracondylar fracture of the femur, 1966-72. Injury. 1974. 6:113–128.
Article23. Schatzker J, Lambert DC. Supracondylar fractures of the femur. Clin Orthop Relat Res. 1979. (138):77–83.
Article24. Schütz M, Müller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: a prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001. 32:Suppl 3. SC48–SC54.
Article25. Schütz M, Müller M, Regazzoni P, et al. Use of the less invasive stabilization system (LISS) in patients with distal femoral (AO33) fractures: a prospective multicenter study. Arch Orthop Trauma Surg. 2005. 125:102–108.
Article26. Vallier HA, Hennessey TA, Sontich JK, Patterson BM, et al. Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am. 2006. 88:846–853.
Article27. Wong MK, Leung F, Chow SP. Treatment of distal femoral fractures in the elderly using a less-invasive plating technique. Int Orthop. 2005. 29:117–120.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Results of Minimally Invasive Plate Osteosynthesis according to Types of Locking Plate in Distal Femoral Fractures
- Clinical Outcomes of Locking Compression Plate Fixation through Minimally Invasive Percutaneous Plate Osteosynthesis in the Treatment of Distal Tibia Fracture
- Analysis of the Result Treated with Locking Compression Plate-Distal Tibia and Zimmer Periarticular Locking Plate in Distal Tibia Fracture
- Minimally Invasive Plate Osteosynthesis with Locking Compression Plate for Distal Femur Fracture
- Minimally Invasive Osteosynthesis with Locking Compression Plate for Distal Tibia Fractures