J Gynecol Oncol.
2013 Jan;24(1):29-36. 10.3802/jgo.2013.24.1.29.
Analysis of para-aortic lymphadenectomy up to the level of the renal vessels in apparent early-stage ovarian cancer
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Ajou University School of Medicine, Suwon, Korea. drchang@ajou.ac.kr
- 2Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, University of California, Irvine School of Medicine, Orange, CA, USA. rbristow@uci.edu
- KMID: 2288558
- DOI: http://doi.org/10.3802/jgo.2013.24.1.29
Abstract
OBJECTIVE
The aim of this study was to evaluate the impact of para-aortic lymphadenectomy up to the renal vessels on the accurate staging in ovarian cancer patients presumed preoperatively to be confined to the ovary.
METHODS
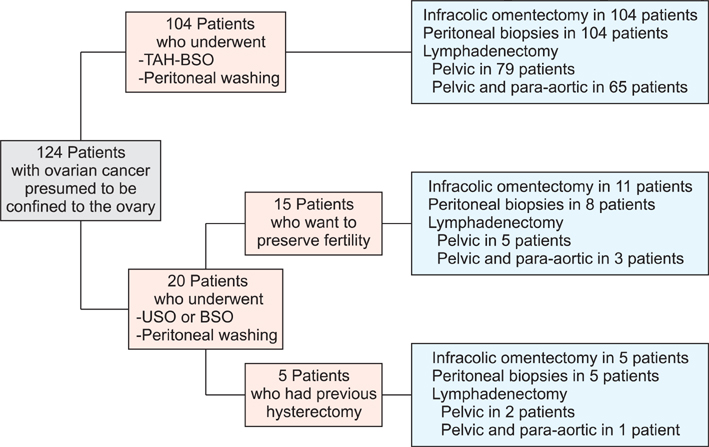
We retrospectively analyzed data on 124 patients with primary epithelial ovarian cancer who were preoperatively thought to have tumor confined to the ovary and underwent primary staging surgery. The distribution of lymph node metastasis and various risk factors for nodal involvement were investigated.
RESULTS
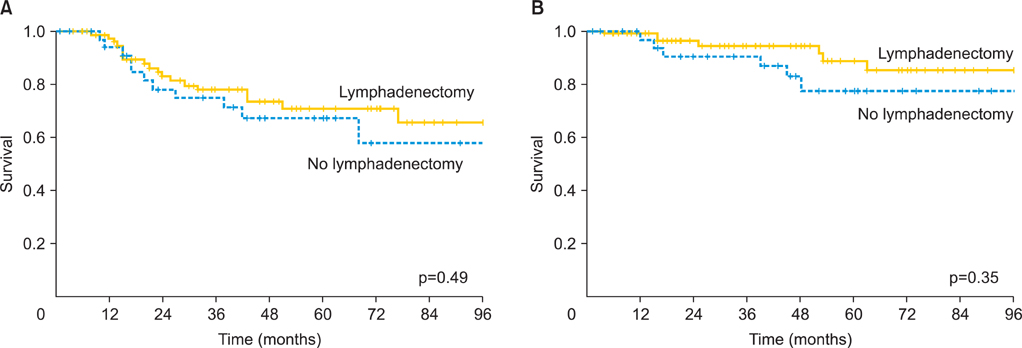
Surgical staging yielded: 87 (70.2%) patients had International Federation of Gynecology and Obstetrics (FIGO) stage I disease and 37 (29.8%) patients had stage II-III disease: 4 IIA, 6 IIB, 9 IIC, 1 IIIA, and 17 IIIC. Eighty-six patients had pelvic lymphadenectomy only and 69 had pelvic and para-aortic lymphadenectomy. Lymph node metastases were found in 17 (24.6%) of 69 patients; 5 (7.2%) patients had lymph node metastasis in the pelvic lymph nodes only, 8 (11.6%) in the para-aortic lymph nodes only, and 4 (5.8%) in both pelvic and para-aortic lymph nodes. Six (8.7%) patients had lymph node metastasis in the para-aortic lymph node above the level of the inferior mesenteric artery. On multivariate analysis, grade 3 tumor (p=0.01) and positive cytology (p=0.03) were independent predictors for lymph node metastasis.
CONCLUSION
A substantial number of patients with apparently early ovarian cancer had upstaged disease. Of patients who underwent lymphadenectomy, some patients had lymph node metastasis above the level of the inferior mesenteric artery. Para-aortic lymphadenectomy up to the renal vessels may detect occult metastasis and be of help in tailoring appropriate adjuvant treatment as well as giving useful information about the prognosis.
MeSH Terms
Figure
Cited by 1 articles
-
Surgical management of ovarian cancer
Suk-Joon Chang
J Korean Med Assoc. 2016;59(3):167-174. doi: 10.5124/jkma.2016.59.3.167.
Reference
-
1. Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011. 61:212–236.2. Chan JK, Munro EG, Cheung MK, Husain A, Teng NN, Berek JS, et al. Association of lymphadenectomy and survival in stage I ovarian cancer patients. Obstet Gynecol. 2007. 109:12–19.3. Shih KK, Chi DS. Maximal cytoreductive effort in epithelial ovarian cancer surgery. J Gynecol Oncol. 2010. 21:75–80.4. Young RC, Decker DG, Wharton JT, Piver MS, Sindelar WF, Edwards BK, et al. Staging laparotomy in early ovarian cancer. JAMA. 1983. 250:3072–3076.5. Le T, Adolph A, Krepart GV, Lotocki R, Heywood MS. The benefits of comprehensive surgical staging in the management of early-stage epithelial ovarian carcinoma. Gynecol Oncol. 2002. 85:351–355.6. Timmers PJ, Zwinderman K, Coens C, Vergote I, Trimbos JB. Lymph node sampling and taking of blind biopsies are important elements of the surgical staging of early ovarian cancer. Int J Gynecol Cancer. 2010. 20:1142–1147.7. Suzuki M, Ohwada M, Yamada T, Kohno T, Sekiguchi I, Sato I. Lymph node metastasis in stage I epithelial ovarian cancer. Gynecol Oncol. 2000. 79:305–308.8. Cass I, Li AJ, Runowicz CD, Fields AL, Goldberg GL, Leuchter RS, et al. Pattern of lymph node metastases in clinically unilateral stage I invasive epithelial ovarian carcinomas. Gynecol Oncol. 2001. 80:56–61.9. Takeshima N, Hirai Y, Umayahara K, Fujiwara K, Takizawa K, Hasumi K. Lymph node metastasis in ovarian cancer: difference between serous and non-serous primary tumors. Gynecol Oncol. 2005. 99:427–431.10. Powless CA, Aletti GD, Bakkum-Gamez JN, Cliby WA. Risk factors for lymph node metastasis in apparent early-stage epithelial ovarian cancer: implications for surgical staging. Gynecol Oncol. 2011. 122:536–540.11. Nomura H, Tsuda H, Susumu N, Fujii T, Banno K, Kataoka F, et al. Lymph node metastasis in grossly apparent stages I and II epithelial ovarian cancer. Int J Gynecol Cancer. 2010. 20:341–345.12. Burghardt E, Girardi F, Lahousen M, Tamussino K, Stettner H. Patterns of pelvic and paraaortic lymph node involvement in ovarian cancer. Gynecol Oncol. 1991. 40:103–106.13. Onda T, Yoshikawa H, Yokota H, Yasugi T, Taketani Y. Assessment of metastases to aortic and pelvic lymph nodes in epithelial ovarian carcinoma: a proposal for essential sites for lymph node biopsy. Cancer. 1996. 78:803–808.14. Morice P, Joulie F, Camatte S, Atallah D, Rouzier R, Pautier P, et al. Lymph node involvement in epithelial ovarian cancer: analysis of 276 pelvic and paraaortic lymphadenectomies and surgical implications. J Am Coll Surg. 2003. 197:198–205.15. Pereira A, Magrina JF, Rey V, Cortes M, Magtibay PM. Pelvic and aortic lymph node metastasis in epithelial ovarian cancer. Gynecol Oncol. 2007. 105:604–608.16. Harter P, Gnauert K, Hils R, Lehmann TG, Fisseler-Eckhoff A, Traut A, et al. Pattern and clinical predictors of lymph node metastases in epithelial ovarian cancer. Int J Gynecol Cancer. 2007. 17:1238–1244.17. Chan J, Fuh K, Shin J, Cheung M, Powell C, Chen LM, et al. The treatment and outcomes of early-stage epithelial ovarian cancer: have we made any progress? Br J Cancer. 2008. 98:1191–1196.18. Cress RD, Bauer K, O'Malley CD, Kahn AR, Schymura MJ, Wike JM, et al. Surgical staging of early stage epithelial ovarian cancer: results from the CDC-NPCR ovarian patterns of care study. Gynecol Oncol. 2011. 121:94–99.19. Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S. FIGO Committee on Gynecologic Oncology. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. Int J Gynaecol Obstet. 2000. 70:209–262.20. Tsumura N, Sakuragi N, Hareyama H, Satoh C, Oikawa M, Yamada H, et al. Distribution pattern and risk factors of pelvic and para-aortic lymph node metastasis in epithelial ovarian carcinoma. Int J Cancer. 1998. 79:526–530.21. Sakuragi N, Yamada H, Oikawa M, Okuyama K, Fujino T, Sagawa T, et al. Prognostic significance of lymph node metastasis and clear cell histology in ovarian carcinoma limited to the pelvis (pT1M0 and pT2M0). Gynecol Oncol. 2000. 79:251–255.22. Grabowski JP, Harter P, Buhrmann C, Lorenz D, Hils R, Kommoss S, et al. Re-operation outcome in patients referred to a gynecologic oncology center with presumed ovarian cancer FIGO I-IIIA after sub-standard initial surgery. Surg Oncol. 2012. 21:31–35.23. Maggioni A, Benedetti Panici P, Dell'Anna T, Landoni F, Lissoni A, Pellegrino A, et al. Randomised study of systematic lymphadenectomy in patients with epithelial ovarian cancer macroscopically confined to the pelvis. Br J Cancer. 2006. 95:699–704.24. Goff BA, Matthews BJ, Wynn M, Muntz HG, Lishner DM, Baldwin LM. Ovarian cancer: patterns of surgical care across the United States. Gynecol Oncol. 2006. 103:383–390.25. Rouzier R, Bergzoll C, Brun JL, Dubernard G, Selle F, Uzan S, et al. The role of lymph node resection in ovarian cancer: analysis of the Surveillance, Epidemiology, and End Results (SEER) database. BJOG. 2010. 117:1451–1458.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of the Para-aortic Lymphadenectomy in Epithelial Ovarian Cancer
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Early ovarian cancer surgery with indocyanine-green-guided targeted compartmental lymphadenectomy (TCL, pelvic part)
- Surgical treatment of early ovarian cancer with compartmental resection of regional lymphatic network and indocyanine-green-guided targeted compartmental lymphadenectomy (TCL, paraaortic part)
- Single-port laparoscopic transperitoneal infrarenal para-aortic lymphadenectomy as part of staging operation for early ovarian cancer and high grade endometrial cancer