J Gynecol Oncol.
2013 Jul;24(3):229-235. 10.3802/jgo.2013.24.3.229.
Prognostic factors and treatment outcome after radiotherapy in cervical cancer patients with isolated para-aortic lymph node metastases
- Affiliations
-
- 1Department of Radiation Oncology, Dongguk University School of Medicine, Gyeongju, Korea.
- 2Department of Radiation Oncology, Ajou University School of Medicine, Suwon, Korea. chunm@ajou.ac.kr
- 3Department of Obstetrics and Gynecology, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2288529
- DOI: http://doi.org/10.3802/jgo.2013.24.3.229
Abstract
OBJECTIVE
The purpose of the present study was to evaluate treatment outcomes and prognostic factors in cervical cancer patients with isolated para-aortic lymph node (PALN) metastases. We especially tried to evaluate PALN factors such as size, site and number.
METHODS
From August 1994 to December 2009, 40 cervical cancer patients with isolated PALN node metastases at initial diagnosis were selected for analysis. Patients underwent both extended field external beam and intracavitary brachytherapy. Fourteen patients received 5-fluorouracil and cisplatin (FP) and 16 patients received weekly concurrent cisplatin. Information of PALN, such as size, site, and number, was founded before PALN radiotherapy.
RESULTS
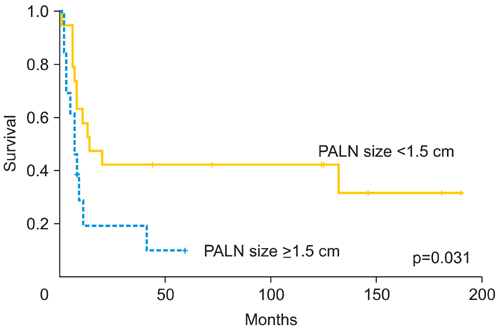
The median follow-up time after primary treatment was 28.5 months (range, 2 to 213 months). The 3-year overall and progression-free survival rate after primary treatment was 44.3% and 31.3%, respectively. In multivariate analysis including tumor stage, performance status, and chemotherapy, FP regimen concurrent chemoradiotherapy was more effective than radiotherapy alone (p=0.030). The 3-year progression-free survival rate was 41.9% and 11.1% in patients with PALN numbers of < or =1 and > or =2, respectively (p=0.008). The 3-year progression-free survival rate was 42.1% and 19.2% in patients with PALN size of <1.5 cm and > or =1.5 cm, respectively (p=0.031).
CONCLUSION
The radiologic features of PALN, such as number or size, can be used to determine prognosis in PALN metastatic cervical cancer patients. Furthermore, FP regimen concurrent chemoradiotherapy was associated with better patient survival than radiotherapy alone. However, more studies are required to confirm possible different treatment outcomes between FP and weekly cisplatin regimens.
MeSH Terms
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001; 94:153–156.2. National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in Oncology [Internet]. Fort Washington, PA: NCCN;2013. cited 2013 May 20. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.3. Sakurai H, Mitsuhashi N, Takahashi M, Akimoto T, Muramatsu H, Ishikawa H, et al. Analysis of recurrence of squamous cell carcinoma of the uterine cervix after definitive radiation therapy alone: patterns of recurrence, latent periods, and prognosis. Int J Radiat Oncol Biol Phys. 2001; 50:1136–1144.4. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–1346.5. Singh AK, Grigsby PW, Rader JS, Mutch DG, Powell MA. Cervix carcinoma, concurrent chemoradiotherapy, and salvage of isolated paraaortic lymph node recurrence. Int J Radiat Oncol Biol Phys. 2005; 61:450–455.6. Rajasooriyar C, Van Dyk S, Bernshaw D, Kondalsamy-Chennakesavan S, Barkati M, Narayan K. Patterns of failure and treatment-related toxicity in advanced cervical cancer patients treated using extended field radiotherapy with curative intent. Int J Radiat Oncol Biol Phys. 2011; 80:422–428.7. Varia MA, Bundy BN, Deppe G, Mannel R, Averette HE, Rose PG, et al. Cervical carcinoma metastatic to para-aortic nodes: extended field radiation therapy with concomitant 5-fluorouracil and cisplatin chemotherapy: a Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys. 1998; 42:1015–1023.8. Grigsby PW, Heydon K, Mutch DG, Kim RY, Eifel P. Long-term follow-up of RTOG 92-10: cervical cancer with positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2001; 51:982–987.9. Kim YS, Shin SS, Nam JH, Kim YT, Kim YM, Kim JH, et al. Prospective randomized comparison of monthly fluorouracil and cisplatin versus weekly cisplatin concurrent with pelvic radiotherapy and high-dose rate brachytherapy for locally advanced cervical cancer. Gynecol Oncol. 2008; 108:195–200.10. Kong TW, Chang SJ, Paek J, Yoo SC, Yoon JH, Chang KH, et al. Comparison of concurrent chemoradiation therapy with weekly cisplatin versus monthly fluorouracil plus cisplatin in FIGO stage IIB-IVA cervical cancer. J Gynecol Oncol. 2012; 23:235–241.11. Zighelboim I, Taylor NP, Powell MA, Gibb RK, Rader JS, Mutch DG, et al. Outcomes in 24 selected patients with stage IVB cervical cancer and excellent performance status treated with radiotherapy and chemotherapy. Radiat Med. 2006; 24:625–630.12. Micke O, Bruns F, Schafer U, Prott FJ, Willich N. The impact of squamous cell carcinoma (SCC) antigen in patients with advanced cancer of uterine cervix treated with (chemo-)radiotherapy. Anticancer Res. 2005; 25:1663–1666.13. Hong JH, Tsai CS, Chang JT, Wang CC, Lai CH, Lee SP, et al. The prognostic significance of pre- and posttreatment SCC levels in patients with squamous cell carcinoma of the cervix treated by radiotherapy. Int J Radiat Oncol Biol Phys. 1998; 41:823–830.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of cervical cancer patients with isolated para-aortic lymph node metastases
- Laparoscopic Para-aortic Lymph Node Dissection in Patients with Gynecologic Malignancy
- Radiotherapy of Para-Aortic Node Metastases in Carcinoma of the Uterine Cervix
- Para-aortic Lymph Node Dissection in Gastric Cancer
- Prognosis of the Patients Showing Metastasis to the Para-aortic or/and Supraclavicular Lymph Nodes at the Time of Diagnosis of Recurrence of the Cervical Cancer