J Breast Cancer.
2014 Sep;17(3):295-298. 10.4048/jbc.2014.17.3.295.
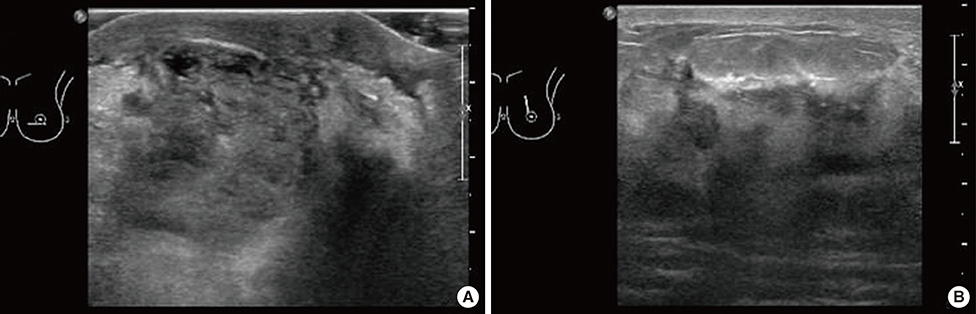
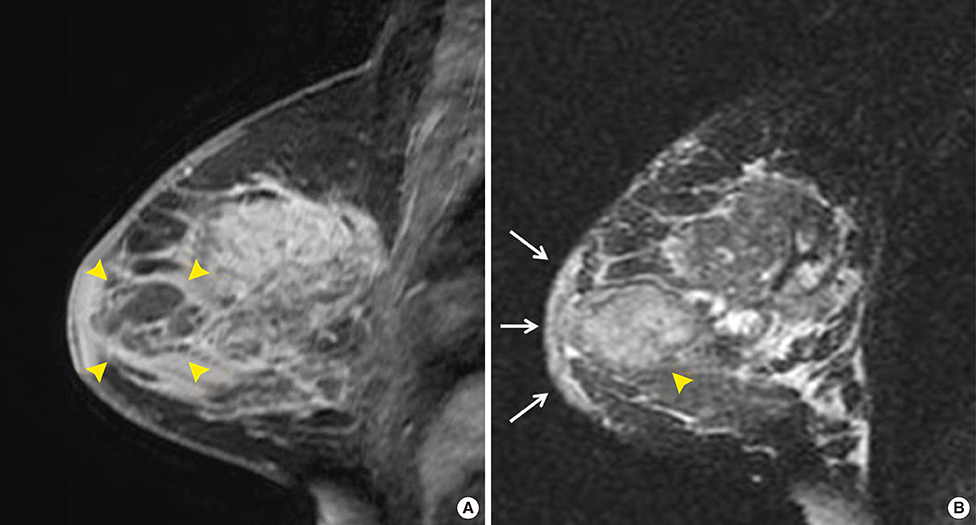
Recurrent Bilateral Breast Abscess Due to Nontuberculous Mycobacterial Infection
- Affiliations
-
- 1Department of Radiology, Inha University Hospital, Inha University College of Medicine, Incheon, Korea. kimyj@inha.ac.kr
- 2Korea Health Promotion Foundation, Seoul, Korea.
- 3Department of Surgery, Inha University Hospital, Inha University College of Medicine, Incheon, Korea.
- 4Department of Pathology, Inha University Hospital, Inha University College of Medicine, Incheon, Korea.
- KMID: 2286359
- DOI: http://doi.org/10.4048/jbc.2014.17.3.295
Abstract
- Since recurrent bilateral breast infection due to nontuberculous mycobacterium (NTM) is rare, its diagnosis is easily overlooked; in addition, complete recovery is often difficult to achieve. We report a case of recurrent bilateral infection in a 35-year-old woman who had completed treatment for NTM. Although various infectious diseases show similar clinical conditions and imaging findings, recurrences should raise suspicion of NTM infection, and this possibility should be considered in differential diagnoses.
MeSH Terms
Figure
Reference
-
1. Kamal RM, Hamed ST, Salem DS. Classification of inflammatory breast disorders and step by step diagnosis. Breast J. 2009; 15:367–380.
Article2. Chirra A. Nontuberculous Mycobacterium infection of the breast. Proceedings of UCLA Healthcare. Accessed December 4th, 2013. Available from: http://www.med.ucla.edu/modules/wfsection/article.php?articleid=567.3. Macadam SA, Mehling BM, Fanning A, Dufton JA, Kowalewska-Grochowska KT, Lennox P, et al. Nontuberculous mycobacterial breast implant infections. Plast Reconstr Surg. 2007; 119:337–344.
Article4. Abdelhadi MS, Bukharie HA. Breast infections in non-lactating women. J Family Community Med. 2005; 12:133–137.5. Tewari M, Shukla HS. Breast tuberculosis: diagnosis, clinical features & management. Indian J Med Res. 2005; 122:103–110.6. Coney PM, Thrush S. Cutaneous Mycobacterium fortuitum complicating breast reconstruction. J Plast Reconstr Aesthet Surg. 2007; 60:1162–1163.
Article7. Vinh DC, Rendina A, Turner R, Embil JM. Breast implant infection with Mycobacterium fortuitum group: report of case and review. J Infect. 2006; 52:e63–e67.
Article8. Rimmer J, Hamilton S, Gault D. Recurrent mycobacterial breast abscesses complicating reconstruction. Br J Plast Surg. 2004; 57:676–678.
Article9. Haiavy J, Tobin H. Mycobacterium fortuitum infection in prosthetic breast implants. Plast Reconstr Surg. 2002; 109:2124–2128.
Article10. Medical Section of the American Lung Association. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Am J Respir Crit Care Med. 1997; 156:S1–S25.11. Betal D, Macneill FA. Chronic breast abscess due to Mycobacterium fortuitum: a case report. J Med Case Rep. 2011; 5:188.
Article12. Cooke FJ, Friedland JS. Spontaneous breast abscess due to Mycobacterium fortuitum. Clin Infect Dis. 1998; 26:760–761.
Article13. Lewis CG, Wells MK, Jennings WC. Mycobacterium fortuitum breast infection following nipple-piercing, mimicking carcinoma. Breast J. 2004; 10:363–365.
Article14. Bengualid V, Singh V, Singh H, Berger J. Mycobacterium fortuitum and anaerobic breast abscess following nipple piercing: case presentation and review of the literature. J Adolesc Health. 2008; 42:530–532.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Abscess due to Mycobacterium Fortuitum: A Case Report
- Huge Abscess due to Mycobacterium Abscessus Infection after Breast Augmentation
- Chronic Large Non Healing Ulcer: Non-Tuberculous Mycobacterial Infection of the Laryngopharynx
- Nontuberculous Mycobacterial Tenosynovitis in the Hand: Two Case Reports with the MR Imaging Findings
- Nontuberculous Mycobacterial Infection after Breast Reconstruction with an Implant: A Case Report