Diabetes Metab J.
2012 Feb;36(1):70-76. 10.4093/dmj.2012.36.1.70.
Prevalence and Correlates of Disordered Sleep in Southeast Asian Indians with Type 2 Diabetes
- Affiliations
-
- 1Department of Endocrinology, Diabetes & Metabolism, Sri Ramachandra University, Chennai, Tamilnadu, India. krishnagseshadri@gmail.com
- 2Sri Ramachandra University, Chennai, Tamilnadu, India.
- KMID: 2281431
- DOI: http://doi.org/10.4093/dmj.2012.36.1.70
Abstract
- BACKGROUND
Sleep disturbances are common in individuals with diabetes. Patients with diabetes have higher rates of insomnia, excessive daytime sleepiness and increased incidence of restless leg syndrome. The purpose of our study was to investigate the prevalence and determine the predictors of sleep dysfunction in patients with type 2 diabetes in a southeast Asian Indian population.
METHODS
We enrolled 120 patients with type 2 diabetes who attended an endocrinology clinic in a tertiary-care hospital. After we collected their demographic data, we recorded their anthropometric measurements. Fasting, postprandial blood glucose values and glycosylated hemoglobin (HbA1c) values were then obtained. Quality of sleep was evaluated in all the patients through the Pittsburgh Sleep Quality Index (PSQI), which is a questionnaire that assesses sleep quality and disturbances over a monthlong period. A Global Sleep Quality score > or =5 discriminates between good and poor sleepers.
RESULTS
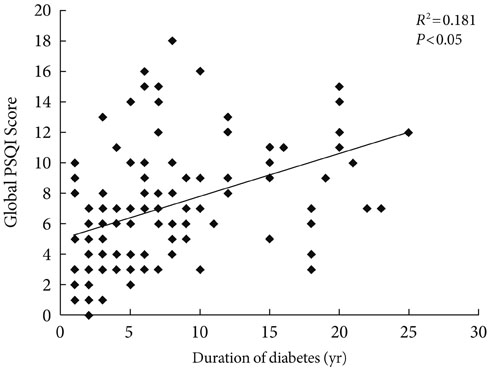
The mean global PSQI score was 7.08 (standard deviation, 3.89), which suggested poor sleep quality in this population. Sixty-nine percent of patients had a global PSQI score > or =5, indicating that they were "poor sleepers." The global PSQI score positively correlated with the duration of diabetes and was also independent of other variables such as age, gender, body mass index, HbA1c, or medications.
CONCLUSION
We found a high prevalence of sleep dysfunction in patients with type 2 diabetes. We also found a significant correlation between duration of diabetes and quality of sleep, independent of other variables. It is important for physicians to address the quality and duration of sleep in patients with type 2 diabetes.
Keyword
MeSH Terms
Figure
Reference
-
1. Tasali E, Mokhlesi B, Van Cauter E. Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest. 2008. 133:496–506.2. Early release of selected estimates based on data from the January-June 2003 National Health Interview Survey. Centers for Disease Control and Prevention. cited 2005 Jan 20. Available from: http://www.cdc.gov/nchs/about/major/nhis/released200312.htm.3. Strohl KP, Novak RD, Singer W, Cahan C, Boehm KD, Denko CW, Hoffstem VS. Insulin levels, blood pressure and sleep apnea. Sleep. 1994. 17:614–618.4. Grunstein RR, Stenlof K, Hedner J, Sjostrom L. Impact of obstructive sleep apnea and sleepiness on metabolic and cardiovascular risk factors in the Swedish Obese Subjects (SOS) Study. Int J Obes Relat Metab Disord. 1995. 19:410–418.5. Stoohs RA, Facchini F, Guilleminault C. Insulin resistance and sleep-disordered breathing in healthy humans. Am J Respir Crit Care Med. 1996. 154:170–174.6. Strohl KP. Diabetes and sleep apnea. Sleep. 1996. 19:S225–S228.7. Ip MS, Lam KS, Ho C, Tsang KW, Lam W. Serum leptin and vascular risk factors in obstructive sleep apnea. Chest. 2000. 118:580–586.8. Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, Kales A, Chrousos GP. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000. 85:1151–1158.9. Elmasry A, Lindberg E, Berne C, Janson C, Gislason T, Awad Tageldin M, Boman G. Sleep-disordered breathing and glucose metabolism in hypertensive men: a population-based study. J Intern Med. 2001. 249:153–161.10. Boyer S, Kapur V. Obstructive sleep apnea: its relevance in the care of diabetic patients. Clin Diabetes. 2002. 20:126–132.11. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989. 28:193–213.12. Fiorentini A, Valente R, Perciaccante A, Tubani L. Sleep's quality disorders in patients with hypertension and type 2 diabetes mellitus. Int J Cardiol. 2007. 114:E50–E52.13. Aloba OO, Adewuya AO, Ola BA, Mapayi BM. Validity of the Pittsburgh Sleep Quality Index (PSQI) among Nigerian university students. Sleep Med. 2007. 8:266–270.14. Einhorn D, Stewart DA, Erman MK, Gordon N, Philis-Tsimikas A, Casal E. Prevalence of sleep apnea in a population of adults with type 2 diabetes mellitus. Endocr Pract. 2007. 13:355–362.15. Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FX, Darcey V, Kuna ST. Sleep AHEAD Research Group. Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009. 32:1017–1019.16. Phillips B, Hening W, Britz P, Mannino D. Prevalence and correlates of restless legs syndrome: results from the 2005 National Sleep Foundation Poll. Chest. 2006. 129:76–80.17. Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D'Agostino RB, Newman AB, Lebowitz MD, Pickering TG. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA. 2000. 283:1829–1836.18. Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000. 342:1378–1384.19. Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O'Connor GT, Boland LL, Schwartz JE, Samet JM. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001. 163:19–25.20. Reichmuth KJ, Austin D, Skatrud JB, Young T. Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med. 2005. 172:1590–1595.21. Hammond EC. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am J Public Health Nations Health. 1964. 54:11–23.22. Wingard DL, Berkman LF, Brand RJ. A multivariate analysis of health-related practices: a nine-year mortality follow-up of the Alameda County Study. Am J Epidemiol. 1982. 116:765–775.23. Vorona RD, Winn MP, Babineau TW, Eng BP, Feldman HR, Ware JC. Overweight and obese patients in a primary care population report less sleep than patients with a normal body mass index. Arch Intern Med. 2005. 165:25–30.24. Nakajima H, Kaneita Y, Yokoyama E, Harano S, Tamaki T, Ibuka E, Kaneko A, Takahashi I, Umeda T, Nakaji S, Ohida T. Association between sleep duration and hemoglobin A1c level. Sleep Med. 2008. 9:745–752.25. Phillips BG, Kato M, Narkiewicz K, Choe I, Somers VK. Increases in leptin levels, sympathetic drive, and weight gain in obstructive sleep apnea. Am J Physiol Heart Circ Physiol. 2000. 279:H234–H237.26. Irwin M, Thompson J, Miller C, Gillin JC, Ziegler M. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. J Clin Endocrinol Metab. 1999. 84:1979–1985.27. Lonnqvist F, Thorne A, Large V, Arner P. Sex differences in visceral fat lipolysis and metabolic complications of obesity. Arterioscler Thromb Vasc Biol. 1997. 17:1472–1480.28. Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004. 141:846–850.29. Wilcox I, McNamara SG, Collins FL, Grunstein RR, Sullivan CE. "Syndrome Z": the interaction of sleep apnoea, vascular risk factors and heart disease. Thorax. 1998. 53:Suppl 3. S25–S28.30. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999. 354:1435–1439.31. Harsch IA, Schahin SP, Radespiel-Troger M, Weintz O, Jahreiss H, Fuchs FS, Wiest GH, Hahn EG, Lohmann T, Konturek PC, Ficker JH. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004. 169:156–162.32. Brooks B, Cistulli PA, Borkman M, Ross G, McGhee S, Grunstein RR, Sullivan CE, Yue DK. Obstructive sleep apnea in obese noninsulin-dependent diabetic patients: effect of continuous positive airway pressure treatment on insulin responsiveness. J Clin Endocrinol Metab. 1994. 79:1681–1685.33. Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T. Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med. 2005. 165:447–452.34. Dawson A, Abel SL, Loving RT, Dailey G, Shadan FF, Cronin JW, Kripke DF, Kline LE. CPAP therapy of obstructive sleep apnea in type 2 diabetics improves glycemic control during sleep. J Clin Sleep Med. 2008. 4:538–542.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Prevalence and Correlates of Disordered Sleep in Southeast Asian Indians with Type 2 Diabetes (Diabetes Metab J 2012;36:70-6)
- Response: Prevalence and Correlates of Disordered Sleep in Southeast Asian Indians with Type 2 Diabetes (Diabetes Metab J 2012;36:70-6)
- Obstructive Sleep Apnea in Women
- Allergic Rhinitis and Sleep-disordered Breathing
- Sleep-disordered breathing in children