Korean J Pain.
2011 Sep;24(3):164-168. 10.3344/kjp.2011.24.3.164.
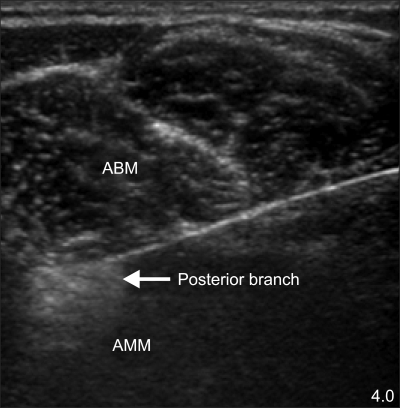
Obturator Nerve Block with Botulinum Toxin Type B for Patient with Adductor Thigh Muscle Spasm: A Case Report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. painfree@snubh.org
- 2Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2278106
- DOI: http://doi.org/10.3344/kjp.2011.24.3.164
Abstract
- Obturator nerve block has been commonly used for pain management to prevent involuntary reflex of the adductor thigh muscles. One of several options for this block is chemical neurolysis. Neurolysis is done with chemical agents. Chemical agents used in the neurolysis of the obturator nerve have been alcohol, phenol, and botulinum toxin. In the current case, a patient with spasticity of the adductor thigh muscle due to cervical cord injury had obturator nerve neurolysis done with botulinum toxin type B (BoNT-B). Most of the previous studies have used BoNT-A with only a few reports that have used BoNT-B. BoNT-B has several advantages and disadvantages over BoNT-A. Thus, we report herein a patient who successfully received obturator nerve neurolysis using BoNT-B to treat adductor thigh muscle spasm.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
A Morphometric Study of the Obturator Nerve around the Obturator Foramen
Se Yeong Jo, Jae Chil Chang, Hack Gun Bae, Jae-Sang Oh, Juneyoung Heo, Jae Chan Hwang
J Korean Neurosurg Soc. 2016;59(3):282-286. doi: 10.3340/jkns.2016.59.3.282.
Reference
-
1. O'Brien CF. Treatment of spasticity with botulinum toxin. Clin J Pain. 2002; 18(6 Suppl):S182–S190. PMID: 12569967.2. Chou R, Peterson K, Helfand M. Comparative efficacy and safety of skeletal muscle relaxants for spasticity and musculoskeletal conditions: a systematic review. J Pain Symptom Manage. 2004; 28:140–175. PMID: 15276195.
Article3. Dressler D, Adib Saberi F. Botulinum toxin: mechanisms of action. Eur Neurol. 2005; 53:3–9. PMID: 15650306.
Article4. Calderón-González R, Calderón-Sepúlveda RF. Clinical treatment (non surgical) of spasticity in cerebral palsy. Rev Neurol. 2002; 34:1–6. PMID: 11988886.5. Ashworth B. Preliminary trial of carisoprodol in multiple sclerosis. Practitioner. 1964; 192:540–542. PMID: 14143329.6. Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. Ophthalmology. 1980; 87:1044–1049. PMID: 7243198.
Article7. Truong DD, Stenner A, Reichel G. Current clinical applications of botulinum toxin. Curr Pharm Des. 2009; 15:3671–3680. PMID: 19925419.
Article8. Grunfeld A, Murray CA, Solish N. Botulinum toxin for hyperhidrosis: a review. Am J Clin Dermatol. 2009; 10:87–102. PMID: 19222249.9. Kharkar S, Ambady P, Yedatore V, Schwartzman RJ. Intramuscular botulinum toxin A (BtxA) in complex regional pain syndrome. Pain Physician. 2011; 14:311–316. PMID: 21587336.10. Lim SJ, Park HJ, Lee SH, Moon DE. Ganglion impar block with botulinum toxin type a for chronic perineal pain -a case report-. Korean J Pain. 2010; 23:65–69. PMID: 20552077.
Article11. Aoki KR. Pharmacology and immunology of botulinum toxin type A. Clin Dermatol. 2003; 21:476–480. PMID: 14759579.
Article12. Comella CL, Jankovic J, Shannon KM, Tsui J, Swenson M, Leurgans S, et al. Comparison of botulinum toxin serotypes A and B for the treatment of cervical dystonia. Neurology. 2005; 65:1423–1429. PMID: 16275831.
Article13. Greene P, Fahn S, Diamond B. Development of resistance to botulinum toxin type A in patients with torticollis. Mov Disord. 1994; 9:213–217. PMID: 8196686.
Article14. Factor SA, Molho ES, Evans S, Feustel PJ. Efficacy and safety of repeated doses of botulinum toxin type B in type A resistant and responsive cervical dystonia. Mov Disord. 2005; 20:1152–1160. PMID: 15954134.
Article15. Callaway JE. Botulinum toxin type B (Myobloc): pharmacology and biochemistry. Clin Dermatol. 2004; 22:23–28. PMID: 15158541.
Article16. Akkaya T, Unlu E, Alptekin A, Gumus HI, Umay E, Cakci A. Neurolytic phenol blockade of the obturator nerve for severe adductor spasticity. Acta Anaesthesiol Scand. 2010; 54:79–85. PMID: 19839948.
Article17. Al-Saleem FH, Ancharski DM, Ravichandran E, Joshi SG, Singh AK, Gong Y, et al. The role of systemic handling in the pathophysiologic actions of botulinum toxin. J Pharmacol Exp Ther. 2008; 326:856–863. PMID: 18539649.
Article18. Figgitt DP, Noble S. Botulinum toxin B: a review of its therapeutic potential in the management of cervical dystonia. Drugs. 2002; 62:705–722. PMID: 11893235.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound Guided both Obturator Nerve Block for Patient with Adductor Thigh Muscle Spasm : A case report
- Inadvertent Breakage of the Spinal Needle during the Obturator Nerve Block for the Transurethral Resection of Bladder Tumor: A case report
- Botulinum Toxin Injection Treatment for Facial Spasm
- Use of Nerve Stimulator for the Obturator Nerve Block
- Obturator Nerve Conduction Study Using Magnetic Stimulation in Healthy Adults