Korean J Pain.
2011 Mar;24(1):36-43. 10.3344/kjp.2011.24.1.36.
The Results of Cervical Nucleoplasty in Patients with Cervical Disc Disorder: A Retrospective Clinical Study of 22 Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Konkuk University Hospital, Seoul, Korea.
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Boramae Hospital, Seoul, Korea.
- 3Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Department of Anesthesiology and Pain Medicine, Chung-Ang University Hospital, Seoul, Korea. paindoctor@paran.com
- KMID: 2278095
- DOI: http://doi.org/10.3344/kjp.2011.24.1.36
Abstract
- BACKGROUND
Nucleoplasty is a minimally invasive spinal surgery using a Coblation(R) technique that creates small voids within the disc. The purpose of this study was to evaluate the efficacy of cervical nucleoplasty in patients with cervical disc disorder.
METHODS
Between March 2008 and December 2009, 22 patients with cervical disc disorders were treated with cervical nucleoplasty after failed conservative treatment. All procedures were performed under local anesthesia, and fluoroscopic guidance and voids were created in the disc with the Perc(TM) DC Spine Wand(TM). Clinical outcomes were evaluated by the Modified Macnab criteria and VAS score at preprocedure, postprocedure 1 month, and 6 months.
RESULTS
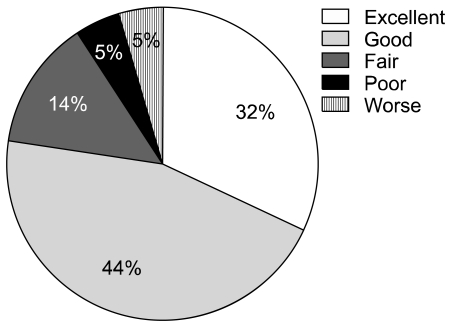
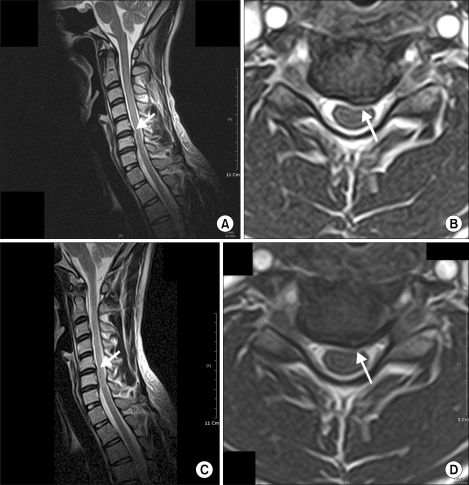
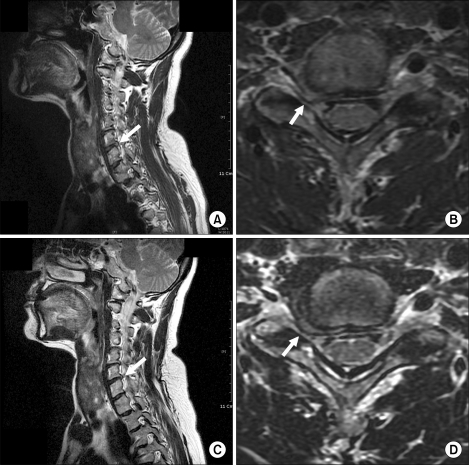
Six patients had one, eight patients had two and eight patients had three discs treated; a total of 46 procedures was performed. Mean VAS reduced from 9.3 at preprocedure to 3.7 at postprocedure 1 month and to 3.4 at postprocedure 6 months. There was no significant complication related to the procedure within the first month. Outcomes were good or excellent in 17/22 (77.3%) cases. Postprocedure magnetic resonance imaging was acquired in two patients after two months showing morphologic evidence of volume reduction of protruded disc material in one patient but not in the other.
CONCLUSIONS
Percutaneous decompression with a nucleoplasty using a Coblation(R) technique in the treatment of cervical disc disorder is a safe, minimally-invasive and less uncomfortable procedure, with an excellent short-term clinical outcome.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Spondylodiscitis after Cervical Nucleoplasty without Any Abnormal Laboratory Findings
Seung Jun Lee, Eun Joo Choi, Francis Sahngun Nahm
Korean J Pain. 2013;26(2):181-185. doi: 10.3344/kjp.2013.26.2.181.
Reference
-
1. Nardi PV, Cabezas D, Cesaroni A. Percutaneous cervical nucleoplasty using coblation technology. Clinical results in fifty consecutive cases. Acta Neurochir Suppl. 2005; 92:73–78. PMID: 15830972.
Article2. Bonaldi G, Baruzzi F, Facchinetti A, Fachinetti P, Lunghi S. Plasma radio-frequency-based diskectomy for treatment of cervical herniated nucleus pulposus: feasibility, safety, and preliminary clinical results. AJNR Am J Neuroradiol. 2006; 27:2104–2111. PMID: 17110676.3. Sharps LS, Isaac Z. Percutaneous disc decompression using nucleoplasty. Pain Physician. 2002; 5:121–126. PMID: 16902662.
Article4. Singh V, Piryani C, Liao K, Nieschulz S. Percutaneous disc decompression using coblation (nucleoplasty) in the treatment of chronic discogenic pain. Pain Physician. 2002; 5:250–259. PMID: 16902650.5. Ro JY, Oh CS, Kim OS, Kim DK, Woo NS, Shin HY. Nucleoplasty in a patient with cervical disc extrusion with radiating pain of an upper extremity. Anesth Pain Med. 2009; 4:203–207.6. Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine. 2003; 28:661–665. PMID: 12671352.
Article7. Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007; 10:7–111. PMID: 17256025.8. Birnbaum K. Percutaneous cervical disc decompression. Surg Radiol Anat. 2009; 31:379–387. PMID: 19190848.
Article9. Calisaneller T, Ozdemir O, Karadeli E, Altinors N. Six months post-operative clinical and 24 hour post-operative MRI examinations after nucleoplasty with radiofrequency energy. Acta Neurochir (Wien). 2007; 149:495–500. PMID: 17431536.
Article10. Singh V. Scientific basis for nucleoplasty. Tech Reg Anesth Pain Manag. 2005; 9:13–24.
Article11. Bhagia SM, Slipman CW, Nirschl M, Isaac Z, El-Abd O, Sharps LS, et al. Side effects and complications after percutaneous disc decompression using coblation technology. Am J Phys Med Rehabil. 2006; 85:6–13. PMID: 16357543.
Article12. Oh WS, Park YO, Shim WS, Wie HW, Woo CH. Psoas abscess and discitis after intradiscal nucleoplasty. Korean J Anesthesiol. 2002; 42:844–849.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous cervical nucleoplasty using the L'DISQ(R) in patients with posterolateral disc extrusion: Three cases report
- Nucleoplasty in a patient with cervical disc extrusion with radiating pain of an upper extremity
- Application of Percutaneous Cervical Nucleoplasty Using the Navigable Disc Decompression Device in Patient of Cervical Herniated Intervertebral Disc: A Case Report
- Retrospective Outcome Evaluation of Cervical Nucleoplasty Using Digital Infrared Thermographic Imaging
- Spondylodiscitis after Cervical Nucleoplasty without Any Abnormal Laboratory Findings