Korean J Pain.
2013 Apr;26(2):181-185. 10.3344/kjp.2013.26.2.181.
Spondylodiscitis after Cervical Nucleoplasty without Any Abnormal Laboratory Findings
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea. hiitsme@snubh.org
- KMID: 1978666
- DOI: http://doi.org/10.3344/kjp.2013.26.2.181
Abstract
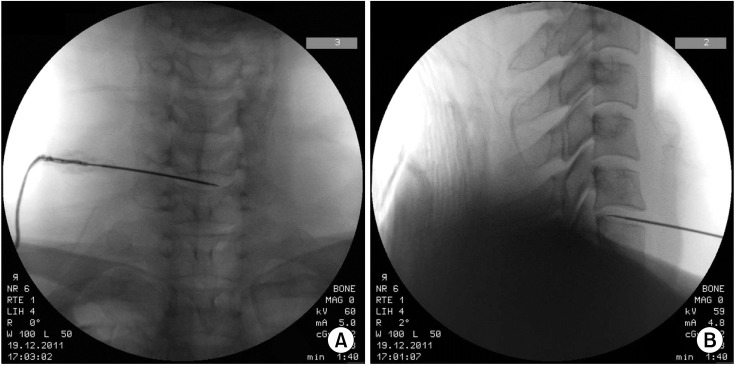
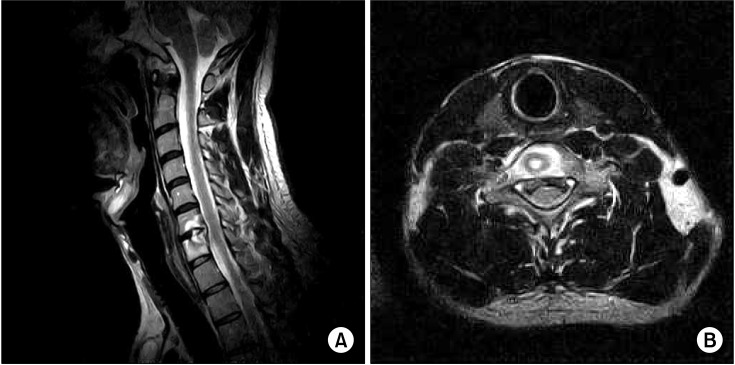
- Infective spondylodiscitis is a rare complication that can occur after interventional spinal procedures, of which symptoms are usually back pain and fever. Early diagnosis of infective spondylodiscitis is critical to start antibiotics and to improve prognosis. Laboratory examinations including complet blood cell count (CBC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) are conventional tools for the early detection of infectious spondylitis. However, we experienced infective spondylodiscitis after cervical nucleoplasty which did not display any laboratory abnormalities, but was diagnosed through an MRI. A patient with cervical disc herniation received nucleoplasty at C5/6 and C6/7. One month later, the patient complained of aggravated pain. There were neither signs of chill nor fever, and the laboratory results appeared normal. However, the MRI findings were compatible with infectious spondylodiscitis at the nucleoplasty site. In conclusion, infectious spondylodiscitis can develop after cervical nucleoplasty without any laboratory abnormalities. Therefore, an MRI should be taken when there is a clinical suspicion for infection in order to not miss complications after interventional procedures, even if the laboratory findings are normal.
MeSH Terms
Figure
Cited by 1 articles
-
Should We Start Treating Chronic Low Back Pain with Antibiotics Rather than with Pain Medications?
Christof Birkenmaier
Korean J Pain. 2013;26(4):327-335. doi: 10.3344/kjp.2013.26.4.327.
Reference
-
1. Di Martino A, Papapietro N, Lanotte A, Russo F, Vadalà G, Denaro V. Spondylodiscitis: standards of current treatment. Curr Med Res Opin. 2012; 28:689–699. PMID: 22435926.
Article2. Jiménez-Mejías ME, de Dios Colmenero J, Sánchez-Lora FJ, Palomino-Nicás J, Reguera JM, García de la Heras J, et al. Postoperative spondylodiskitis: etiology, clinical findings, prognosis, and comparison with nonoperative pyogenic spondylodiskitis. Clin Infect Dis. 1999; 29:339–345. PMID: 10476739.
Article3. Bonaldi G, Baruzzi F, Facchinetti A, Fachinetti P, Lunghi S. Plasma radio-frequency-based diskectomy for treatment of cervical herniated nucleus pulposus: feasibility, safety, and preliminary clinical results. AJNR Am J Neuroradiol. 2006; 27:2104–2111. PMID: 17110676.4. Chen F, Lü G, Kang Y, Ma Z, Lu C, Wang B, et al. Mucormycosis spondylodiscitis after lumbar disc puncture. Eur Spine J. 2006; 15:370–376. PMID: 16328227.
Article5. Lotfinia I, Vahedi P. Late-onset post-diskectomy tuberculosis at the same operated lumbar level: case report and review of literature. Eur Spine J. 2010; 19(Suppl 2):S226–S232. PMID: 20446000.
Article6. Bavinzski G, Schoeggl A, Trattnig S, Standhardt H, Dietrich W, Reddy M, et al. Microsurgical management of postoperative disc space infection. Neurosurg Rev. 2003; 26:102–107. PMID: 12962295.
Article7. Schulitz KP, Assheuer J. Discitis after procedures on the intervertebral disc. Spine. 1994; 19:1172–1177. PMID: 8059276.
Article8. Mustard RA Jr, Bohnen JM, Haseeb S, Kasina R. C-reactive protein levels predict postoperative septic complications. Arch Surg. 1987; 122:69–73. PMID: 3800652.
Article9. Sim SE, Ko ES, Kim DK, Kim HK, Kim YC, Shin HY. The results of cervical nucleoplasty in patients with cervical disc disorder: a retrospective clinical study of 22 patients. Korean J Pain. 2011; 24:36–43. PMID: 21390177.
Article10. Ozuna RM, Delamarter RB. Pyogenic vertebral osteomyelitis and postsurgical disc space infections. Orthop Clin North Am. 1996; 27:87–94. PMID: 8539056.
Article11. Rohde V, Meyer B, Schaller C, Hassler WE. Spondylodiscitis after lumbar discectomy. Incidence and a proposal for prophylaxis. Spine. 1998; 23:615–620. PMID: 9530794.12. Meyer B, Schaller K, Rohde V, Hassler W. The C-reactive protein for detection of early infections after lumbar microdiscectomy. Acta Neurochir. 1995; 136:145–150. PMID: 8748845.
Article13. Bircher MD, Tasker T, Crawshaw C, Mulholland RC. Discitis following lumbar surgery. Spine. 1988; 13:98–102. PMID: 3381147.
Article14. Kwon SC, Kim SJ, Shin HS, Park SK. Erythrocyte sedimentation rate, C-reactive protein, and white blood cell count after lumbar discectomy. J Korean Neurosurg Soc. 1998; 27:1508–1511.15. Citak M, Backhaus M, Kälicke T, Hilal Z, Muhr G, Frangen TM. Myths and facts of spondylodiscitis: an analysis of 183 cases. Acta Orthop Belg. 2011; 77:535–538. PMID: 21954765.16. Gerometta A, Bittan F, Rodriguez Olaverri JC. Postoperative spondilodiscitis. Int Orthop. 2012; 36:433–438. PMID: 22307558.
Article17. Zarghooni K, Röllinghoff M, Sobottke R, Eysel P. Treatment of spondylodiscitis. Int Orthop. 2012; 36:405–411. PMID: 22143315.
Article18. Palestro CJ, Love C, Miller TT. Infection and musculoskeletal conditions: imaging of musculoskeletal infections. Best Pract Res Clin Rheumatol. 2006; 20:1197–1218. PMID: 17127204.19. Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics. 1999; 22:758–765. PMID: 10465488.
Article20. Maiuri F, Iaconetta G, Gallicchio B, Manto A, Briganti F. Spondylodiscitis. Clinical and magnetic resonance diagnosis. Spine. 1997; 22:1741–1746. PMID: 9259785.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nucleoplasty in a patient with cervical disc extrusion with radiating pain of an upper extremity
- Percutaneous cervical nucleoplasty using the L'DISQ(R) in patients with posterolateral disc extrusion: Three cases report
- Cervical Spondylodiscitis Caused by Candida Albicans in Non-Immunocompromised Patient
- A case of infective endocarditis presented as cervical spondylodiscitis
- Application of Percutaneous Cervical Nucleoplasty Using the Navigable Disc Decompression Device in Patient of Cervical Herniated Intervertebral Disc: A Case Report