Chonnam Med J.
2012 Apr;48(1):73-75. 10.4068/cmj.2012.48.1.73.
A Case of Duodenal Anisakiasis with Duodenal Ulcer
- Affiliations
-
- 1Department of Internal Medicine, Seonam University College of Medicine, Seonam University Namkwang Hospital, Gwangju, Korea. lsmed@hanmail.net
- 221C Hana Medical Clinic, Mokpo, Korea.
- KMID: 2274887
- DOI: http://doi.org/10.4068/cmj.2012.48.1.73
Abstract
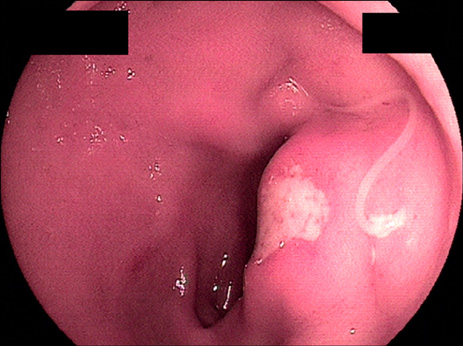
- Humans can be incidentally parasitized by third-stage larvae of Anisakis species following the ingestion of raw or undercooked seafood. Acute gastric anisakiasis is one of the most frequently encountered complaints in Korea. However, duodenal anisakiasis with duodenal ulcer had not been reported in Korea, despite the habit of eating raw fish. In this case, a 47-year-old man was hospitalized because of sharp epigastric pain and repeated vomiting after eating raw fish 3 days previously. On admission, esophagogastroduodenoscopic examination revealed an active duodenal bulb ulcer. At 5 mm away from the ulcer margin, a whitish linear worm was found with half of its body penetrating the duodenal mucosa. Herein, we report this case of duodenal anisakiasis accompanied by duodenal ulcer.
Keyword
MeSH Terms
Figure
Reference
-
1. Van Thiel P, Kuipers FC, Roskam RT. A nematode parasitic to herring, causing acute abdominal syndromes in man. Trop Geogr Med. 1960. 12:97–113.2. Kang DB, Oh JT, Park WC, Lee JK. Small bowel obstruction caused by acute invasive enteric anisakiasis. Korean J Gastroenterol. 2010. 56:192–195.
Article3. Lee EJ, Kim YC, Jeong HG, Lee OJ. The mucosal changes and influencing factors in upper gastrointestinal anisakiasis: analysis of 141 cases. Korean J Gastroenterol. 2009. 53:90–97.4. Choi SJ, Lee JC, Kim MJ, Hur GY, Shin SY, Park HS. The clinical characteristics of Anisakis allergy in Korea. Korean J Intern Med. 2009. 24:160–163.
Article5. Okada F, Hiratsuka H. Araki T, Tsuji M, Katsu K, Hirata I, editors. Gastric anisakiasis. Clinical parasitology for endoscopist [Japanese]. 2000. Tokyo: Igaku-tosho-shuppan;98–102.6. Takeuchi K, Hanai H, Iida T, Suzuki S, Isobe S. A bleeding gastric ulcer on a vanishing tumor caused by anisakiasis. Gastrointest Endosc. 2000. 52:549–551.
Article7. Lee CM, Choi JY, Kim JH. Intestinal obstruction caused by anisakiasis. J Korean Surg Soc. 2008. 74:154–156.8. Matsui T, Iida M, Murakami M, Kimura Y, Fujishima M, Yao Y, et al. Intestinal anisakiasis: clinical and radiologic features. Radiology. 1985. 157:299–302.
Article9. Audicana MT, Ansotegui IJ, de Corres LF, Kennedy MW. Anisakis simplex: dangerous--dead and alive? Trends Parasitol. 2002. 18:20–25.10. Nakaji K. Enteric anisakiasis which improved with conservative treatment. Intern Med. 2009. 48:573.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Resolution of Duodenal Obstruction Caused by Duodenal Ulcer after the Eradication of Helicobacter pylori Infection
- Three Cases of Coexistence of Gastric Cancer and Duodenal Ulcer
- A Case of Coexistence of Gastric Cancer and Duodenal Ulcer
- Duodenal Anisakiasis Presenting as Bowel Obstruction and Fistula Formation: A Case Report
- Bezoar in pseudodiverticulum of the duodenal bulb