Ann Rehabil Med.
2015 Apr;39(2):253-261. 10.5535/arm.2015.39.2.253.
Can Motor Evoked Potentials Be an Objective Parameter to Assess Extremity Function at the Acute or Subacute Stroke Stage?
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Chonbuk National University Medical School, Jeonju, Korea. mhko@jbnu.ac.kr
- 2Research Institute of Clinical Medicine of Chonbuk National University and Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2273047
- DOI: http://doi.org/10.5535/arm.2015.39.2.253
Abstract
OBJECTIVE
To investigate whether motor evoked potential (MEP) amplitude ratio measurements are sufficiently objective to assess functional activities of the extremities. We also delineated the distribution between the presence or absence of MEPs and the Medical Research Council (MRC) scale for muscle strength of the extremities.
METHODS
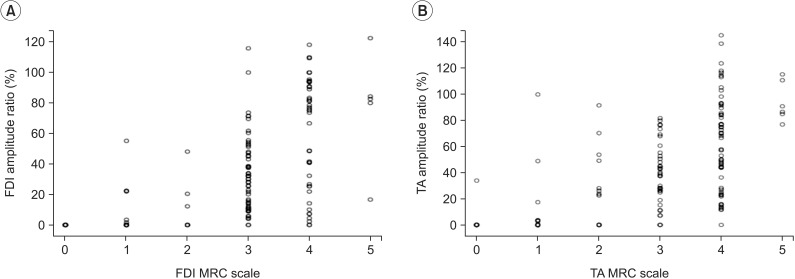
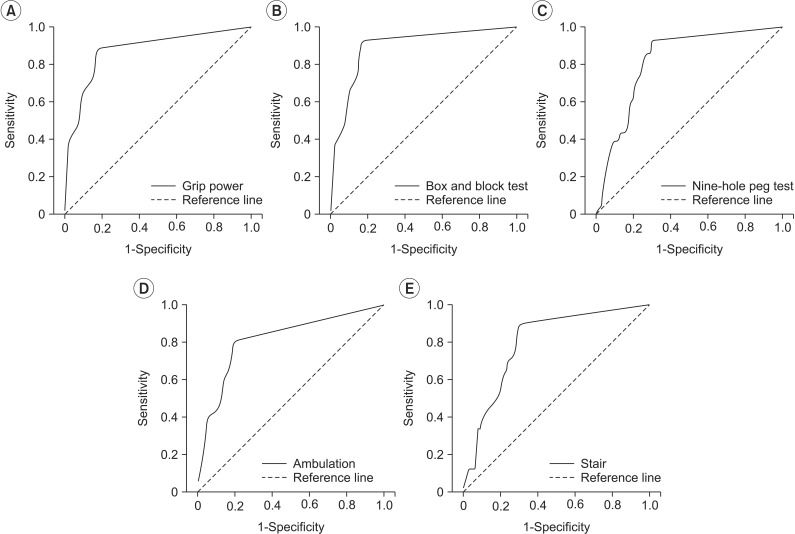
We enrolled 183 patients with first-ever unilateral hemiplegia after stroke. The MEP parameters were amplitude ratio (amplitude of affected side/amplitude of unaffected side) recorded at the first dorsal interosseous (FDI) and tibialis anterior (TA) muscles. We performed frequency analyses using the MRC scale for muscle strength and the presence or absence of evoked MEPs. Change on the MRC scale, hand function tests (HFTs), and the Modified Barthel Index (MBI) subscore were compared between the evoked MEP and absent MEP groups using the independent t-test. Receiver operating characteristic curves were used to determine the optimal cutoff scores for the MEP amplitude ratio using the HFT results and MBI subscores. Correlations between the MEP amplitude ratio and the MRC scale, HFTs, and MBI subscore were analyzed.
RESULTS
About 10% of patients with MRC scale grades 0-2 showed evoked MEPs at the FDI muscle, and 4% of patients with MRC scale grades 3-5 did not show MEPs. About 18% of patients with MRC scale grades 0-2 showed evoked MEPs at the TA muscle, and 4% of patients with MRC scale grades 3-5 did not show MEPs. MEP amplitude increased with increasing MRC scale grade. The evoked MEP group had more significant changes on the MRC scale, HFT, and the climbing stair score on the MBI than those in the group without MEPs. Larger MEP amplitude ratios were observed in patients who had more difficulty with the HFTs and ambulation. The MEP amplitude ratio was significantly correlated with the MRC scale, HFT, and MBI subscore.
CONCLUSION
We conclude that the MEP amplitude ratio may be useful to predict functional status of the extremities in patients who suffered stroke.
MeSH Terms
Figure
Cited by 2 articles
-
Prediction of Motor Recovery Using Quantitative Parameters of Motor Evoked Potential in Patients With Stroke
Jae Yong Jo, Ahee Lee, Min Su Kim, Eunhee Park, Won Hyuk Chang, Yong-Il Shin, Yun-Hee Kim
Ann Rehabil Med. 2016;40(5):806-815. doi: 10.5535/arm.2016.40.5.806.Diagnostic Challenge of Diffusion Tensor Imaging in a Patient With Hemiplegia After Traumatic Brain Injury
Hye Eun Shin, Hoon Chang Suh, Si Hyun Kang, Kyung Mook Seo, Don-Kyu Kim, Hae-Won Shin
Ann Rehabil Med. 2017;41(1):153-157. doi: 10.5535/arm.2017.41.1.153.
Reference
-
1. Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009; 8:741–754. PMID: 19608100.
Article2. Hendricks HT, van Limbeek J, Geurts AC, Zwarts MJ. Motor recovery after stroke: a systematic review of the literature. Arch Phys Med Rehabil. 2002; 83:1629–1637. PMID: 12422337.
Article3. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988; 19:1497–1500. PMID: 3201508.
Article4. Escudero JV, Sancho J, Bautista D, Escudero M, Lopez-Trigo J. Prognostic value of motor evoked potential obtained by transcranial magnetic brain stimulation in motor function recovery in patients with acute ischemic stroke. Stroke. 1998; 29:1854–1859. PMID: 9731608.
Article5. Talelli P, Greenwood RJ, Rothwell JC. Arm function after stroke: neurophysiological correlates and recovery mechanisms assessed by transcranial magnetic stimulation. Clin Neurophysiol. 2006; 117:1641–1659. PMID: 16595189.
Article6. Trompetto C, Assini A, Buccolieri A, Marchese R, Abbruzzese G. Motor recovery following stroke: a transcranial magnetic stimulation study. Clin Neurophysiol. 2000; 111:1860–1867. PMID: 11018503.
Article7. van Kuijk AA, Pasman JW, Hendricks HT, Zwarts MJ, Geurts AC. Predicting hand motor recovery in severe stroke: the role of motor evoked potentials in relation to early clinical assessment. Neurorehabil Neural Repair. 2009; 23:45–51. PMID: 18794218.
Article8. Son SY, Park SH, Seo JH, Ko MH. Correlation of the motor evoked potentials amplitude and hand function of the affected side in stroke. J Korean Acad Rehabil Med. 2011; 35:34–41.9. Thickbroom GW, Byrnes ML, Archer SA, Mastaglia FL. Motor outcome after subcortical stroke: MEPs correlate with hand strength but not dexterity. Clin Neurophysiol. 2002; 113:2025–2029. PMID: 12464343.
Article10. Lee JJ, Jung HY. The correlation of hemiplegic upper limb recovery with SEP and MEP in subjects with a stroke. J Korean Acad Rehabil Med. 2008; 32:512–517.11. Hendricks HT, Pasman JW, van Limbeek J, Zwarts MJ. Motor evoked potentials of the lower extremity in predicting motor recovery and ambulation after stroke: a cohort study. Arch Phys Med Rehabil. 2003; 84:1373–1379. PMID: 13680577.12. Kim C, Jeong J. The significance of motor evoked potentials as a prognostic factor in the early stage of stroke patients. J Korean Acad Rehabil Med. 1999; 23:1213–1220.13. Lim KB, Kim JA. Activity of daily living and motor evoked potentials in the subacute stroke patients. Ann Rehabil Med. 2013; 37:82–87. PMID: 23525518.
Article14. Piron L, Piccione F, Tonin P, Dam M. Clinical correlation between motor evoked potentials and gait recovery in poststroke patients. Arch Phys Med Rehabil. 2005; 86:1874–1878. PMID: 16181957.
Article15. Pizzi A, Carrai R, Falsini C, Martini M, Verdesca S, Grippo A. Prognostic value of motor evoked potentials in motor function recovery of upper limb after stroke. J Rehabil Med. 2009; 41:654–660. PMID: 19565160.
Article16. Pennisi G, Rapisarda G, Bella R, Calabrese V, Maertens De Noordhout A, Delwaide PJ. Absence of response to early transcranial magnetic stimulation in ischemic stroke patients: prognostic value for hand motor recovery. Stroke. 1999; 30:2666–2670. PMID: 10582994.17. Lee SY, Lim JY, Kang EK, Han MK, Bae HJ, Paik NJ. Prediction of good functional recovery after stroke based on combined motor and somatosensory evoked potential findings. J Rehabil Med. 2010; 42:16–20. PMID: 20111839.
Article18. van Hedel HJ, Murer C, Dietz V, Curt A. The amplitude of lower leg motor evoked potentials is a reliable measure when controlled for torque and motor task. J Neurol. 2007; 254:1089–1098. PMID: 17431701.
Article19. Jang SH. The role of the corticospinal tract in motor recovery in patients with a stroke: a review. NeuroRehabilitation. 2009; 24:285–290. PMID: 19458437.
Article20. Thickbroom GW, Byrnes ML, Mastaglia FL. A model of the effect of MEP amplitude variation on the accuracy of TMS mapping. Clin Neurophysiol. 1999; 110:941–943. PMID: 10400209.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Motor Evoked Potentials and Somatosensory Evoked Potentials of Upper and Lower Extremities for Prediction of Functional Recovery in Stroke
- The Significance of Motor Evoked Potentials as a Prognostic Factor in the Early Stage of Stroke Patients
- Motor Evoked Potentials of Upper and Lower Extremities by Magnetic Stimulation in Hemiparesis
- Comparison of Diffusion Tensor Tractography and Motor Evoked Potentials for the Estimation of Clinical Status in Subacute Stroke
- Association Between Evoked Potentials and Balance Recovery in Subacute Hemiparetic Stroke Patients