Brain Neurorehabil.
2013 Mar;6(1):9-16. 10.12786/bn.2013.6.1.9.
Effectiveness of Fiberoptic Endoscopic Evaluation of Swallowing (FEES) in Patients with Swallowing Disorders -A Systematic Review-
- Affiliations
-
- 1The National Evidence-based Healthcare Collaborating Agency, Center for New Health Technology Assessment, Korea.
- 2Department of Otolaryngology-Head and Neck Surgery, School of Medicine, The Catholic University of Korea, Korea.
- 3Yonsei Rehabilitation Clinic, Korea.
- 4Department of Otolaryngology-Head and Neck Surgery, Kyung Hee University School of Medicine, Korea.
- 5Division of Gastroenterology, Department of Internal Medicine, School of Medicine, The Catholic University of Korea, Korea.
- 6Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. yunkim@skku.edu
- KMID: 2270734
- DOI: http://doi.org/10.12786/bn.2013.6.1.9
Abstract
OBJECTIVE
The objective of this systematic review is to evaluate the safety and effectiveness of fiberoptic endoscopic evaluation of swallowing (FEES) for dysphagia patients. METHOD: We performed a systematic review of the literature. We searched Ovid-Medline(R), EMBASE(R) and Cochrane library(R) and Eight domestic databases including KoreaMed up to 19 April 2010. In addition, we added hand search. Searches were conducted without language restriction. We identified ten studies that met our eligibility criteria. Two reviewers independently extracted prespecified data from each study. Also reviewers assessed quality of each study. The qualities of these studies were assessed according to Scottish Intercollegiate Guidelines Network (SIGN) tool.
RESULTS
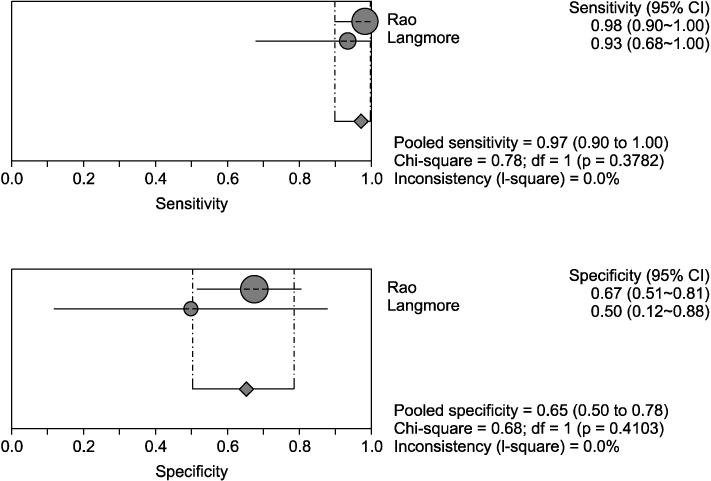
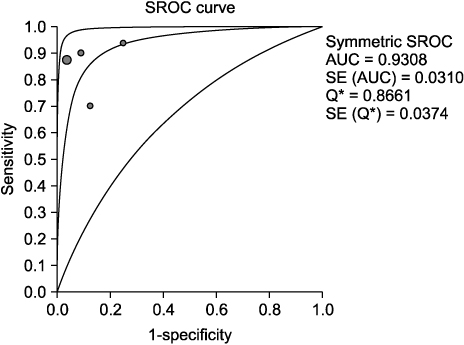
Ten studies (nine diagnostic evaluation studies and one case series) were identified. The complication rate of FEES was 6% which was reported only one study as nose bleeding that did not need further treatment. The effectiveness of FEES was evaluated based on diagnostic accuracy, agreement rate with videofluoroscopy as a reference test. The sensitivities of FEES were 0.87~1.0 (penetration), 0.22~0.96 (aspiration), 0.68~0.91 (pharyngeal residue), and 0.75 (premature spillage) respectively. Specificities of FEES were 0.75~1.0 (penetration), 0.88~1.0 (aspiration), 0.86~1.0 (pharyngeal residue), and 0.56 (premature spillage) respectively. Agreement rate with VFFS were 85~100% (penetration), 82.3~100% (aspiration), 80~89.3% (pharyngeal residues), and 60.7% (premature spillage) respectively. There was no evidence of statistical heterogeneity. The body of evidence as a whole suggests a grade C for FEES.
CONCLUSION
FEES is considered as a safe and effective test in patients with dyspahgia and grade C evidence based on existing studies.
Keyword
MeSH Terms
Figure
Reference
-
1. Spinelli KS, Easterling CS, Shaker R. Radiographic evaluation of complex dysphagic patients: comparison with videoendoscopic technique. Curr Gastroenterol Rep. 2002. 4:187–192.2. Kim YH, Han TR, Jung HY, Chun MH, Lee JM, Kim DY, Paik NJ, Park SW, Kim MW, Pyun SB, Yoo WK, Shin YI, Kim IS, Han SJ, Kim DY, Ohn SH, Chang WH, Lee KH, Kwon SU, Yoon BW. Clinical practice guideline for Stroke rehabilitation in Korea. Brain Neurorehabil. 2009. 2:1–38.3. Murray J, Langmore SE, Ginsberg S, Dosite A. The significance of accumulated oropharyngeal secretions and swallowing frequency in predicting aspiration. Dysphagia. 1996. 11:99–103.4. Horner J, Massy EW. Silent aspiration following stroke. Neurology. 1988. 38:317–319.5. Schroter-Morasch H, Bartalome G, Troppmann N, Ziegier W. Values and limitation of pharyngoloryngoscopy (transnasal, transoral) in patients with dysphagia. Folia Phoniatr Logop. 1999. 51:172–182.6. Willging JP. Functional endoscopic evaluation of swallowing safety. Curr Opin Otolaryngol Head Neck Surg. 1997. 5:387–390.7. Langmore SE, Schatz K, Olsen N. Fiberoptic endoscopic examination of swallowing safety: a new procedure. Dysphagia. 1988. 2:216–219.8. Kelly AM, Leslie P, Beale T, Payten C, Drinnan MJ. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: does examination type influence perception of pharyngeal residue severity? Clin Otolaryngol. 2006. 31:425–432.9. Park YH. Management of oropharyngeal dysphagia. Korean J Otolaryngol-Head Neck Surg. 2003. 46:997–1004.10. Warnecke T, Teismann I, Oelenberg S, Hamacher C, Ringelstein EB, Schabitz WR, Dziewas R. The safety of fiberoptic endoscopic evaluation of swallowing in acute stroke patients. Stroke. 2009. 40:482–486.11. Duncan PW, Zorowitz R, Bates B, Choi JY, Glasberg JJ, Graham GD, Katz RC, Lamberty K, Reker D. Management of adult stroke rehabilitation care: a clinical practice guideline. Stroke. 2005. 36:e100–e143.12. Scottish Intercollegiate Guidelines Network. SIGN 50: a guideline developer's handbook. Accessed 27 December 2011. http://www.sign.ac.uk/pdf/sign50.pdf.13. Kaye GM, Zorowitz RD, Baredes S. Role of flexible layngoscopy in evaluating aspiration. Ann Otol Rhinol Laryngol. 1997. 106:705–709.14. Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991. 100:678–681.15. Madden C, Fenton J, Hughes J, Timon C. Comparison between videofluoroscopy and milk-swallow endoscopy in the assessment of swallowing function. Clin Otolaryngol Allied Sci. 2000. 25:504–506.16. Perie S, Laccourreye L, Flahault A, Hazebroucq V, Chaussade S, Guily JLS. Role of videoendoscopy in assessment of pharyngeal function in oropharyngeal dysphagia: comparison with videofluoroscopy and manometry. Laryngoscope. 1998. 108:1712–1716.17. Rao N, Brady SL, Chaudhuri G, Donzelli JJ, Wesling MW. Gold-standard? Analysis of the videofluoroscopic and fiberoptic endoscopic swallow examinations. J Appl Res. 2003. 3:89–96.18. Leder SB, Bayar S, Sasaki CT, Salem RR. Fiberoptic endoscopic evaluation of swallowing in assessing aspiration after transhiatal esophagectomy. J Am Coll Surg. 2007. 205:581–585.19. Wu CH, Hsiao TY, Chen JC, Chang YC, Lee SY. Evaluation of swallowing safety with fiberoptic endoscope: comparison with videofluoroscopic technique. Laryngoscope. 1997. 107:396–401.20. Kelly AM, Drinnan MJ, Leslie P. Assessing penetration and aspiration: how do videofluoroscopy and fiberoptic endoscopic evaluation of swallowing compare? Laryngoscope. 2007. 117:1723–1727.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and successful visual biofeedback therapy using fiberoptic endoscopic evaluation of swallowing in a young adult patient with psychogenic dysphagia: a case report
- The Usefulness of Flexible Endoscopic Evaluation of Swallowing in Head and Neck Cancer Patients
- Instrumental Assessment of Swallowing
- Detection of pharyngeal perforation during fiberoptic endoscopic evaluation of swallowing in a person with cervical spinal cord injury in the intensive care unit: a case report
- Development of a New Scale for Pharyngeal Residue Using Videofluoroscopic Swallowing Study and Fiberoptic Endoscopy