Ann Rehabil Med.
2014 Dec;38(6):734-741. 10.5535/arm.2014.38.6.734.
Clinical Characteristics Associated With Aspiration or Penetration in Children With Swallowing Problem
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. keepwiz@gmail.com
- KMID: 2267082
- DOI: http://doi.org/10.5535/arm.2014.38.6.734
Abstract
OBJECTIVE
To evaluate demographic characteristics of children with suspected dysphagia who underwent videofluoroscopic swallowing study (VFSS) and to identify factors related to penetration or aspiration.
METHODS
Medical records of 352 children (197 boys, 155 girls) with suspected dysphagia who were referred for VFSS were reviewed retrospectively. Clinical characteristics and VFSS findings were analyzed using univariate and multivariate analyses.
RESULTS
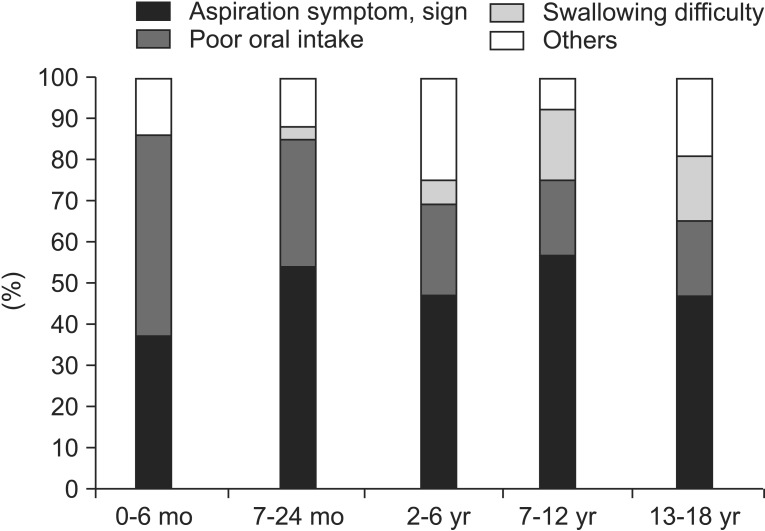
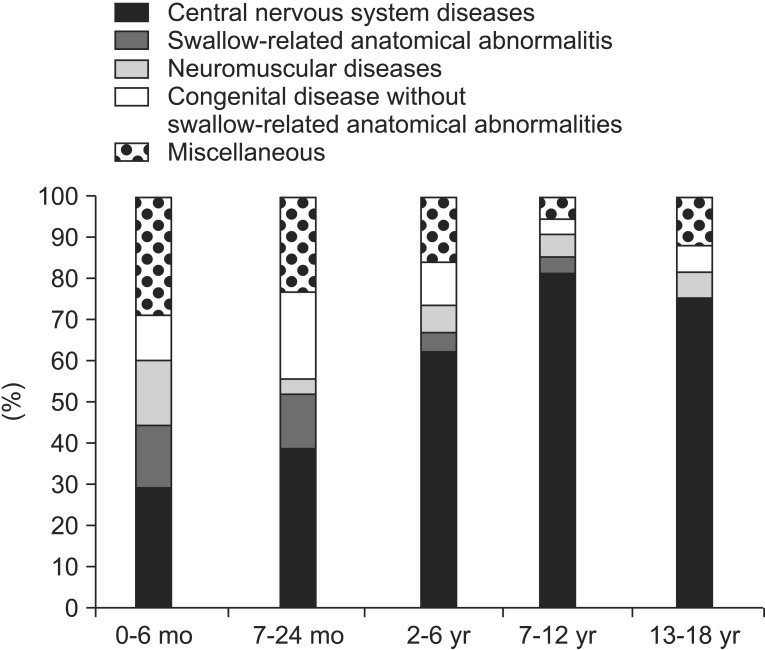
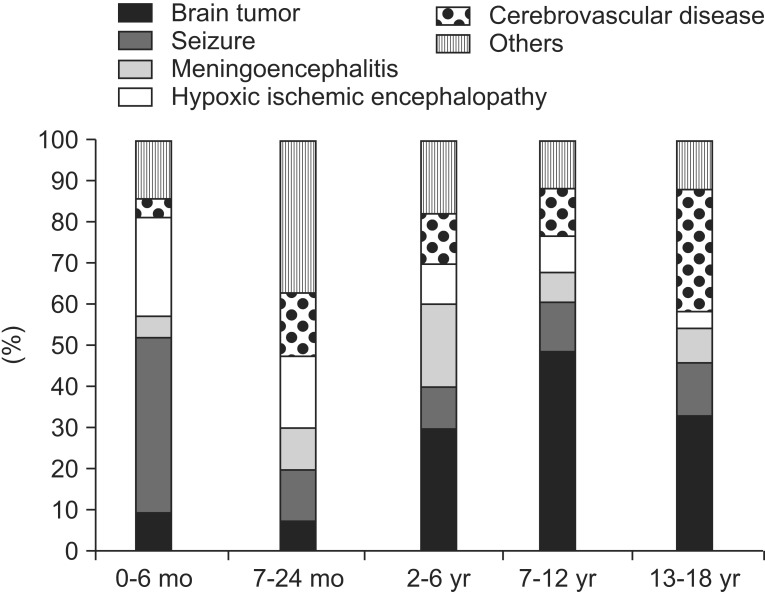
Almost half of the subjects (n=175, 49%) were under 24 months of age with 62 subjects (18%) born prematurely. The most common condition associated with suspected dysphagia was central nervous system (CNS) disease. Seizure was the most common CNS disorder in children of 6 months old or younger. Brain tumor was the most important one for school-age children. Aspiration symptoms or signs were the major cause of referral for VFSS in children except for infants of 6 months old or where half of the subjects showed poor oral intake. Penetration or aspiration was observed in 206 of 352 children (59%). Subjects under two years of age who were born prematurely at less than 34 weeks of gestation were significantly (p=0.026) more likely to show penetration or aspiration. Subjects with congenital disorder with swallow-related anatomical abnormalities had a higher percentage of penetration or aspiration with marginal statistical significance (p=0.074). Multivariate logistic regression analysis revealed that age under 24 months and an unclear etiology for dysphagia were factors associated with penetration or aspiration.
CONCLUSION
Subjects with dysphagia in age group under 24 months with preterm history and unclear etiology for dysphagia may require VFSS. The most common condition associated with dysphagia in children was CNS disease.
MeSH Terms
-
Brain Neoplasms
Central Nervous System
Central Nervous System Diseases
Child*
Congenital, Hereditary, and Neonatal Diseases and Abnormalities
Deglutition Disorders
Deglutition*
Fluoroscopy
Humans
Infant
Infant, Newborn
Infant, Premature
Logistic Models
Medical Records
Multivariate Analysis
Pediatrics
Pneumonia, Aspiration
Pregnancy
Referral and Consultation
Retrospective Studies
Seizures
Figure
Cited by 1 articles
-
Development of a Dysphagia Screening Test for Preterm Infants (DST-PI)
Kyoung Moo Lee, Young Tak Seo
Ann Rehabil Med. 2017;41(3):434-440. doi: 10.5535/arm.2017.41.3.434.
Reference
-
1. Linscheid TR. Behavioral treatments for pediatric feeding disorders. Behav Modif. 2006; 30:6–23. PMID: 16332643.
Article2. Field D, Garland M, Williams K. Correlates of specific childhood feeding problems. J Paediatr Child Health. 2003; 39:299–304. PMID: 12755939.
Article3. Jones PM. Feeding disorders in children with multiple handicaps. Dev Med Child Neurol. 1989; 31:404–406. PMID: 2666208.
Article4. Loughlin GM. Respiratory consequences of dysfunctional swallowing and aspiration. Dysphagia. 1989; 3:126–130. PMID: 2700953.
Article5. Newman LA, Keckley C, Petersen MC, Hamner A. Swallowing function and medical diagnoses in infants suspected of dysphagia. Pediatrics. 2001; 108:E106. PMID: 11731633.
Article6. Rommel N, De Meyer AM, Feenstra L, Veereman-Wauters G. The complexity of feeding problems in 700 infants and young children presenting to a tertiary care institution. J Pediatr Gastroenterol Nutr. 2003; 37:75–84. PMID: 12827010.
Article7. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Kirmeyer S, et al. Births: final data for 2005. Natl Vital Stat Rep. 2007; 56:1–103. PMID: 18277471.8. Hiorns MP, Ryan MM. Current practice in paediatric videofluoroscopy. Pediatr Radiol. 2006; 36:911–919. PMID: 16552584.
Article9. DeMatteo C, Matovich D, Hjartarson A. Comparison of clinical and videofluoroscopic evaluation of children with feeding and swallowing difficulties. Dev Med Child Neurol. 2005; 47:149–157. PMID: 15739718.
Article10. Kramer SS, Eicher PM. The evaluation of pediatric feeding abnormalities. Dysphagia. 1993; 8:215–224. PMID: 8359041.
Article11. Delaney AL, Arvedson JC. Development of swallowing and feeding: prenatal through first year of life. Dev Disabil Res Rev. 2008; 14:105–117. PMID: 18646020.
Article12. Logemann JA. Manual for the videofluorographic study of swallowing. 2nd ed. Austin: Pro-Ed;1993.13. Lefton-Greif MA. Pediatric dysphagia. Phys Med Rehabil Clin N Am. 2008; 19:837–851, ix. PMID: 18940644.
Article14. Ozaki K, Kagaya H, Yokoyama M, Saitoh E, Okada S, Gonzalez-Fernandez M, et al. The risk of penetration or aspiration during videofluoroscopic examination of swallowing varies depending on food types. Tohoku J Exp Med. 2010; 220:41–46. PMID: 20046051.
Article15. Uhm KE, Yi SH, Chang HJ, Cheon HJ, Kwon JY. Videofluoroscopic swallowing study findings in full-term and preterm infants with Dysphagia. Ann Rehabil Med. 2013; 37:175–182. PMID: 23705111.
Article16. Lee JH, Chang YS, Yoo HS, Ahn SY, Seo HJ, Choi SH, et al. Swallowing dysfunction in very low birth weight infants with oral feeding desaturation. World J Pediatr. 2011; 7:337–343. PMID: 22015726.
Article17. Mercado-Deane MG, Burton EM, Harlow SA, Glover AS, Deane DA, Guill MF, et al. Swallowing dysfunction in infants less than 1 year of age. Pediatr Radiol. 2001; 31:423–428. PMID: 11436889.
Article18. Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008; 97:61–67. PMID: 18052999.
Article19. Love RJ, Hagerman EL, Taimi EG. Speech performance, dysphagia and oral reflexes in cerebral palsy. J Speech Hear Disord. 1980; 45:59–75. PMID: 7354631.
Article20. Sachdeva R, Hussain E, Moss MM, Schmitz ML, Ray RM, Imamura M, et al. Vocal cord dysfunction and feeding difficulties after pediatric cardiovascular surgery. J Pediatr. 2007; 151:312–315. 315.e1–315.e2. PMID: 17719946.
Article21. Skoretz SA, Flowers HL, Martino R. The incidence of dysphagia following endotracheal intubation: a systematic review. Chest. 2010; 137:665–673. PMID: 20202948.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between the Type of Laryngeal Penetration and Severity of Tracheal Aspiration in the Brain Injured
- The Relation Between the Presence of Aspiration or Penetration and the Clinical Indicators of Dysphagia in Poststroke Survivors
- Fluoroscopic Swallowing Study in Elderly Patients Admitted to a Geriatric Hospital and a Long-Term Care Facility
- Effect of Hyaluronic Acid Injection for Dysphagia Due to Vocal Fold Paralysis after Influenza Infection – A Case Report
- Investigation of the Swallowing Parameters Related to the Aspiration Risk in the Elderly over 65 Years Old