Ann Rehabil Med.
2012 Aug;36(4):488-495. 10.5535/arm.2012.36.4.488.
Reliability of the Supraspinatus Muscle Thickness Measurement by Ultrasonography
- Affiliations
-
- 1Department of Rehabilitation Medicine, Bundang Jesaeng General Hospital, Seongnam 463-774, Korea. hislyw@gmail.com
- KMID: 2266719
- DOI: http://doi.org/10.5535/arm.2012.36.4.488
Abstract
OBJECTIVE
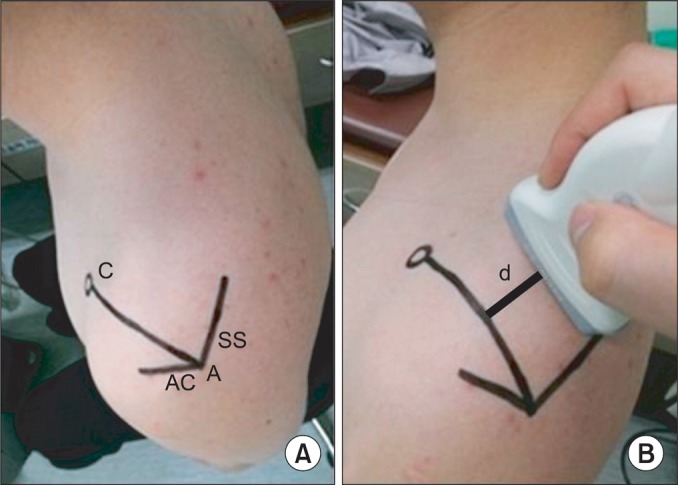
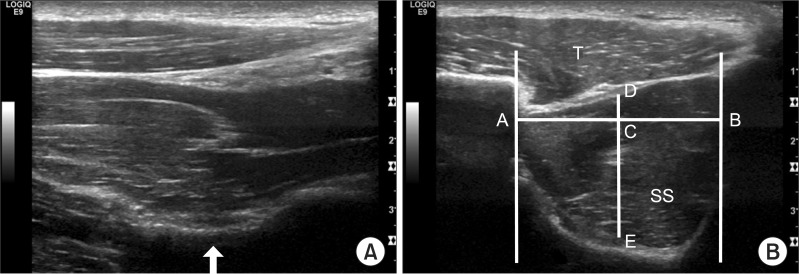
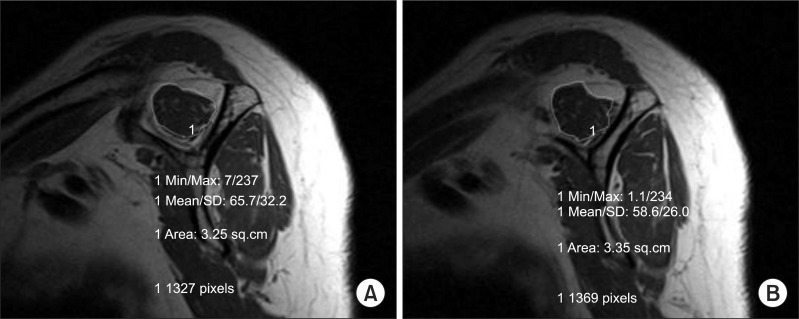
To assess the intrarater and interrater reliability of the supraspinatus thickness measured by ultrasonography (US) in normal subjects and to identify the relationship between the supraspinatus thickness measured by US and cross sectional area (CSA) of the supraspinatus muscle by magnetic resonance imaging (MRI) in hemiplegic patients. METHOD: We examined 20 shoulders of normal subjects and 10 shoulders of hemiplegic patients. In normal subjects, one examiner measured the supraspinatus thickness twice by US at the scapular notch and another examiner measured the supraspinatus thickness several days later. The intrarater and interrater reliability of supraspinatus thickness measurements were then evaluated. In hemiplegic patients, the supraspinatus thickness at the scapular notch was measured by US in affected side and compared with CSA of the supraspinatus muscle at the scapular notch and the Y-view of MRI.
RESULTS
One examiner's supraspinatus thickness measurement average was 1.72+/-0.21 cm and 1.74+/-0.24 cm, and the other examiner's supraspinatus thickness measurement average was 1.74+/-0.22 cm in normal subjects. Intraclass correlation coefficients of intrarater and interrater examination were 0.91 and 0.88, respectively. For hemiplegic patients, the supraspinatus thickness measured by US was 1.66+/-0.13 cm and CSA by MRI was 4.83+/-0.88 cm2 at the Y-view and 5.61+/-1.19 cm2 at the scapular notch. The Pearson Correlation Coefficient between the supraspinatus thickness at the scapular notch and the CSA at the Y-view was 0.72 and that between the supraspinatus thickness and CSA at the scapular notch was 0.76.
CONCLUSION
The supraspinatus thickness measurement by US is a reliable method and is positively correlated with the CSA of the supraspinatus muscle in MRI in hemiplegic patients. Therefore, supraspinatus thickness measurement by US can be used in the evaluation of muscle atrophy and to determine therapeutic effects in hemiplegic patients.
Figure
Cited by 1 articles
-
Quantitative Measurement of Muscle Atrophy and Fat Infiltration of the Supraspinatus Muscle Using Ultrasonography After Arthroscopic Rotator Cuff Repair
Yong Ki Kim, Eun Seok Choi, Keon Tae Kim, Jung Ro Yoon, Sang Han Chae
Ann Rehabil Med. 2018;42(2):260-269. doi: 10.5535/arm.2018.42.2.260.
Reference
-
1. Rockwood CA, Matsen FA. The shoulder. 1998. Philadelphia: Saunders;p. 233–276.2. Wilk KE, Arrigo C. Current concepts in the rehabilitation of the athletic shoulder. J Orthop Sports Phys Ther. 1993; 18:365–378. PMID: 8348138.
Article3. Reinold MM, Macrina LC, Wilk KE, Fleisig GS, Dun S, Barrentine SW, Ellerbusch MT, Andrews JR. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J Athl Train. 2007; 42:464–469. PMID: 18174934.4. Bjorkenheim JM. Structure and function of the rabbit's supraspinatus muscle after resection of its tendon. Acta Orthop Scand. 1989; 60:461–463. PMID: 2816325.5. Thomazeau H, Boukobza E, Morcet N, Chaperon J, Langlais F. Prediction of rotator cuff repair results by magnetic resonance imaging. Clin Orthop Relat Res. 1997; 344:275–283. PMID: 9372778.
Article6. Chaco J, Wolf E. Subluxation of the glenohumeral joint in hemiplegia. Am J Phys Med. 1971; 50:139–143. PMID: 5579071.7. Boettcher CE, Ginn KA, Cathers I. Which is the optimal exercise to strengthen supraspinatus? Med Sci Sports Exerc. 2009; 41:1979–1983. PMID: 19812522.
Article8. Takeda Y, Kashiwaguchi S, Endo K, Matsuura T, Sasa T. The most effective exercise for strengthening the supraspinatus muscle: evaluation by magnetic resonance imaging. Am J Sports Med. 2002; 30:374–381. PMID: 12016078.9. Gerber C, Blumenthal S, Curt A, Werner CM. Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Shoulder Elbow Surg. 2007; 16:815–820. PMID: 17931906.
Article10. Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand. 1996; 67:264–268. PMID: 8686465.
Article11. Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008; 190:1105–1111. PMID: 18356462.
Article12. Katayose M, Magee DJ. The cross-sectional area of suprapinatus as measured by diagnostic ultrasound. J Bone Joint Surg Br. 2001; 83:565–568. PMID: 11380133.13. Yanagisawa O, Dohi M, Okuwaki T, Tawara N, Niitsu M, Takahashi H. Appropriate slice location to assess maximal cross-sectional area of individual rotator cuff muscles in normal adults and athletes. Magn Reson Med Sci. 2009; 8:65–71. PMID: 19571498.
Article14. Juul-Kristensen B, Bojsen-Møller F, Holst E, Ekdahl C. Comparision of muscle sizes and moment arms of two rotator cuff muscles measured by ultrasonography and magnetic resonance imaging. Eur J Ultrasound. 2000; 11:161–173. PMID: 10874191.15. Lehtinen JT, Tingart MJ, Apreleva M, Zurakowski D, Palmer W, Warner JJ. Practical assessment of rotator cuff muscle volumes using shoulder MRI. Acta Orthop Scand. 2003; 74:722–729. PMID: 14763706.
Article16. Lieber RL. Skeletal muscle structure and function. 1992. 1st ed. Baltimore: Williams & Wilkins;p. 1–48.17. Kim YS, Heo NY, Kim MW. The test-retest reliability of supraspinatus cross-sectional area measurement by sonography. Ann Rehabil Med. 2011; 35:524–528. PMID: 22506168.
Article18. Collin C, Wade D. Assessing motor impairment after stroke: a pilot reliability study. J Neurol Neurosurg Psychiatry. 1990; 53:576–579. PMID: 2391521.
Article19. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994; 304:78–83. PMID: 8020238.20. Basmajian JV. Muscles alive: their functions revealed by electromyography. 1978. 4th ed. Baltimore: Williams & Wilkins;p. 421–485.21. Yoon TS, Kim DH, Park JW, Kwon BS, Ryu KH, Lee HJ, Park NK, Shim JH. Causes of the hemiplegic shoulder pain. J Korean Acad Rehabil Med. 2010; 34:158–162.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intra and Inter-Rater Measurement Reliability of Tibialis Anterior Muscle (TA) Thickness using the Ultrasonography Spring Gauge Technique
- The Test-Retest Reliability of Supraspinatus Cross-Sectional Area Measurement by Sonography
- Quantitative Measurement of Muscle Atrophy and Fat Infiltration of the Supraspinatus Muscle Using Ultrasonography After Arthroscopic Rotator Cuff Repair
- Diagnosis of Partial Thickness Tear of Supraspinatus Tendon Using Dynamic Ultrasonography Under Resisted Scaption Position
- The Impact of Vibration Exercises on Shoulder Muscle Thickness