Ann Rehabil Med.
2013 Oct;37(5):750-754. 10.5535/arm.2013.37.5.750.
Recurrent Cerebral Infarction Caused by Mobile Aortic Arch Thrombus Refractory to Warfarin Therapy
- Affiliations
-
- 1Department of Rehabilitation Medicine, Chungnam National University School of Medicine, Daejeon, Korea. asyoung@cnuh.co.kr
- 2Department of Rehabilitation Medicine, Konyang University School of Medicine, Daejeon, Korea.
- KMID: 2266598
- DOI: http://doi.org/10.5535/arm.2013.37.5.750
Abstract
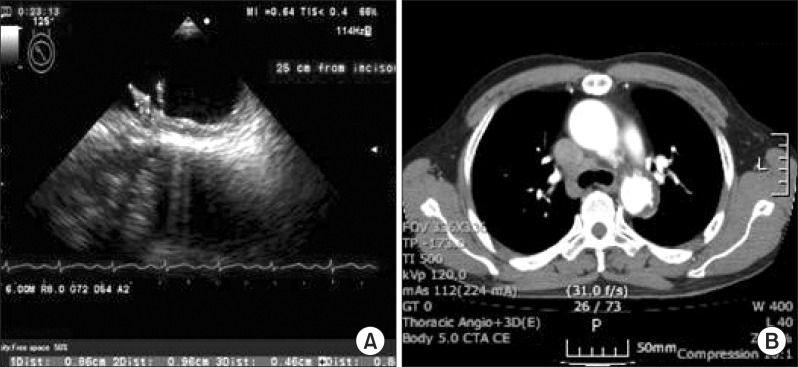
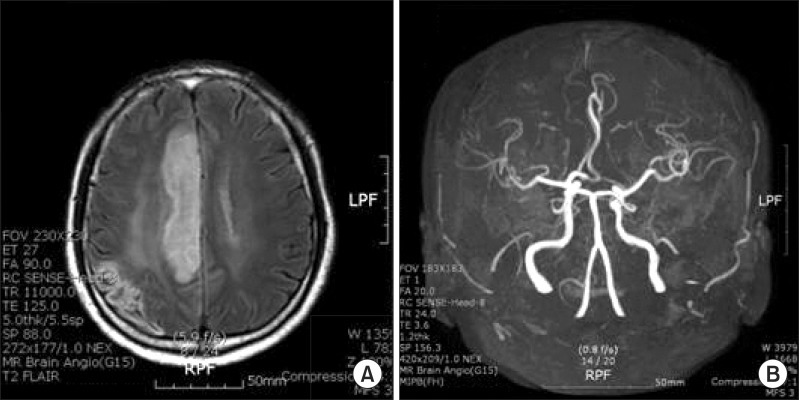
- The mobile thrombus in the aortic arch is a rare condition, which becomes rarer when associated with cerebral infarction, resulting in disabling complications. Transesophageal echocardiography is useful for detecting the source of thrombi in the heart and aortic arch. Here, we report a case of a patient who suffered from recurrent cerebral infarction four times during the previous 18 months due to mobile thrombus in the aortic arch despite anticoagulant therapy. The thrombus with rocking motion (9.6 and 8 mm) was laid in the top of the aortic arch, and surgical resection was not allowed due to the location. We began anticoagulation therapy initially with heparin followed by a combination of warfarin, aspirin, and atorvastatin with an international normalized ratio between 2 and 3. The size of the aortic thrombi was significantly decreased by 3 mm and stabilized after 18 months.
Keyword
MeSH Terms
Figure
Reference
-
1. Khatibzadeh M, Mitusch R, Stierle U, Gromoll B, Sheikhzadeh A. Aortic atherosclerotic plaques as a source of systemic embolism. J Am Coll Cardiol. 1996; 27:664–669. PMID: 8606279.
Article2. Machleder HI, Takiff H, Lois JF, Holburt E. Aortic mural thrombus: an occult source of arterial thromboembolism. J Vasc Surg. 1986; 4:473–478. PMID: 3773130.
Article3. Gagliardi JM, Batt M, Khodja RH, Le bas P. Mural thrombus of the aorta. Ann Vasc Surg. 1988; 2:201–204. PMID: 3191002.
Article4. Laperche T, Laurian C, Roudaut R, Steg PG. Mobile thromboses of the aortic arch without aortic debris: a transesophageal echocardiographic finding associated with unexplained arterial embolism. The Filiale Echocardiographie de la Societe Francaise de Cardiologie. Circulation. 1997; 96:288–294. PMID: 9236447.5. Tunick PA, Kronzon I. Protruding atherosclerotic plaque in the aortic arch of patients with systemic embolization: a new finding seen by transesophageal echocardiography. Am Heart J. 1990; 120:658–660. PMID: 2389701.
Article6. Meissner I, Khandheria BK, Sheps SG, Schwartz GL, Wiebers DO, Whisnant JP, et al. Atherosclerosis of the aorta: risk factor, risk marker, or innocent bystander? A prospective population-based transesophageal echocardiography study. J Am Coll Cardiol. 2004; 44:1018–1024. PMID: 15337213.7. Amarenco P, Cohen A, Tzourio C, Bertrand B, Hommel M, Besson G, et al. Atherosclerotic disease of the aortic arch and the risk of ischemic stroke. N Engl J Med. 1994; 331:1474–1479. PMID: 7969297.
Article8. Song IW, Hong GR, Cho JH, Jun SY, Son CW, Lee SH, et al. A case of huge thrombus in the aortic arch with cerebrovascular embolization. J Cardiovasc Ultrasound. 2009; 17:148–150. PMID: 20661342.
Article9. Williams GM, Harrington D, Burdick J, White RI. Mural thrombus of the aorta: an important, frequently neglected cause of large peripheral emboli. Ann Surg. 1981; 194:737–744. PMID: 7305488.10. Tsilimparis N, Hanack U, Pisimisis G, Yousefi S, Wintzer C, Ruckert RI. Thrombus in the non-aneurysmal, non-atherosclerotic descending thoracic aorta: an unusual source of arterial embolism. Eur J Vasc Endovasc Surg. 2011; 41:450–457. PMID: 21145267.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Embolic Infarction Caused by Aortic Arch Thrombus with Iron Deficiency Anemia
- Cerebral Infarction Caused by Floating Thoracic aortic Thrombus in Young Male
- Floating Thrombus in Aortic Arch
- Acute Abdominal Mobile Aortic Thrombus Post Chemotherapy: Two Cases Reports
- A Case of Huge Thrombus in the Aortic Arch with Cerebrovascular Embolization