Ann Dermatol.
2010 Aug;22(3):319-322. 10.5021/ad.2010.22.3.319.
A Case of Tubular Apocrine Adenoma with Syringocystadenoma Papilliferum that Developed in a Nevus Sebaceus
- Affiliations
-
- 1Department of Dermatology, Eulji Medical Center, College of Medicine, Eulji University, Seoul, Korea. ssjmdderma@eulji.ac.kr
- 2Department of Pathology, Eulji Medical Center, College of Medicine, Eulji University, Seoul, Korea.
- KMID: 2265367
- DOI: http://doi.org/10.5021/ad.2010.22.3.319
Abstract
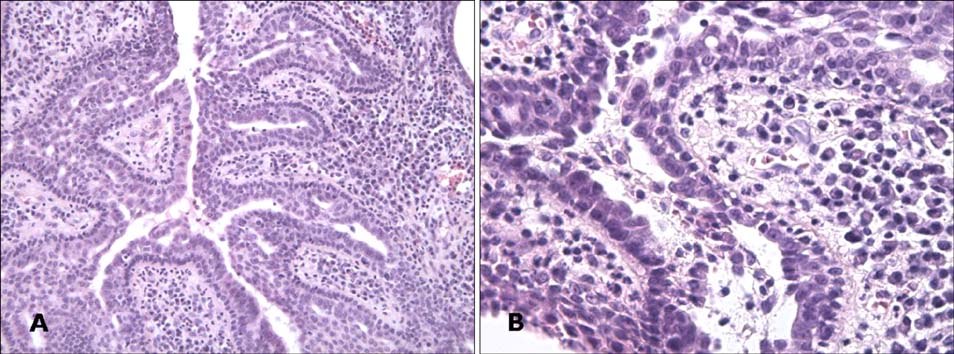
- Tubular apocrine adenoma (TAA) is a very rare sweat gland tumor. TAA and syringocystadenoma papilliferum (SCAP) rarely develop together in a nevus sebaceus (NS). Herein, we report on a 40-year-old Korean woman with TAA associated with SCAP that developed in a NS located on the scalp.
Figure
Cited by 3 articles
-
Syringocystadenoma Papilliferum of the Back Combined with a Tubular Apocrine Adenoma
Hyun Joo Lee, Eujin Cho, Min Ho Kim, Sang Hyun Cho, Jeong Deuk Lee
Ann Dermatol. 2011;23(Suppl 2):S151-S154. doi: 10.5021/ad.2011.23.S2.S151.Syringocystadenoma Papilliferum in Co-existence with Tubular Apocrine Adenoma on the Calf
Jung Hee Yoon, Hyo Hyun Ahn, Young Chul Kye, Soo Hong Seo
Ann Dermatol. 2011;23(Suppl 2):S175-S178. doi: 10.5021/ad.2011.23.S2.S175.Syringocystadenocarcinoma Papilliferum: A Case Report and Review of the Literature
Kyoung Geun Lee, Won Choi, Joon Soo Lim, Hyung Jin Hahn, Ki Bum Myung, Seung Hyun Cheong
Ann Dermatol. 2019;31(5):559-562. doi: 10.5021/ad.2019.31.5.559.
Reference
-
1. Landry M, Winkelmann RK. An unusual tubular apocrine adenoma. Arch Dermatol. 1972. 105:869–879.
Article2. Fischer TL. Tubular apocrine adenoma. Arch Dermatol. 1973. 107:137.
Article3. Umbert P, Winkelmann RK. Tubular apocrine adenoma. J Cutan Pathol. 1976. 3:75–87.
Article4. Toribio J, Zulaica A, Peteiro C. Tubular apocrine adenoma. J Cutan Pathol. 1987. 14:114–117.
Article5. Ansai S, Watanabe S, Aso K. A case of tubular apocrine adenoma with syringocystadenoma papilliferum. J Cutan Pathol. 1989. 16:230–236.
Article6. Ishiko A, Shimizu H, Inamoto N, Nakmura K. Is tubular apocrine adenoma a distinct clinical entity? Am J Dermatopathol. 1993. 15:482–487.
Article7. Aktepe F, Demir Y, Dilek FH. Tubular apocrine adenoma in association with syringocystadenoma papilliferum. Dermatol Online J. 2003. 9:7.
Article8. Ahn BK, Park YK, Kim YC. A case of tubular apocrine adenoma with syringocystadenoma papilliferum arising in nevus sebaceus. J Dermatol. 2004. 31:508–510.
Article9. Lee CK, Jang KT, Cho YS. Tubular apocrine adenoma with syringocystadenoma papilliferum arising from the external auditory canal. J Laryngol Otol. 2005. 119:1004–1006.
Article10. Yamane N, Kato N, Yanagi T, Osawa R. Naevus sebaceus on the female breast accompanied with a tubular apocrine adenoma and a syringocystadenoma papilliferum. Br J Dermatol. 2007. 156:1397–1399.
Article11. Cribier B, Scrivener Y, Grosshans E. Tumors arising in nevus sebaceus: a study of 596 cases. J Am Acad Dermatol. 2000. 42:263–268.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Cases of Nevus Sebaceus of Jandassohn Associated with Tubular Apocrine Adenoma
- A Case of Nevus Sebaceus associated with Tubular Apocrine Adenoma and Apocrine Poroma
- Syringocystadenoma Papilliferum in Co-existence with Tubular Apocrine Adenoma on the Calf
- Three Cases Showing Combined Features of Syringocystadenoma Papilliferum andTubular Apocrine Adenoma Superimposed on Nevus Sebaceus
- Development of Six Tumors in a Sebaceus Nevus of Jadassohn: Report of a Case