Anat Cell Biol.
2013 Sep;46(3):171-176. 10.5115/acb.2013.46.3.171.
Histological assessment of the palatal mucosa and greater palatine artery with reference to subepithelial connective tissue grafting
- Affiliations
-
- 1Department of Anatomy and Orofacial Development, School of Dentistry, Chosun University, Gwangju, Korea. hjbkim@chosun.ac.kr
- KMID: 2263142
- DOI: http://doi.org/10.5115/acb.2013.46.3.171
Abstract
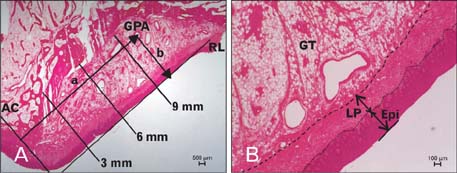
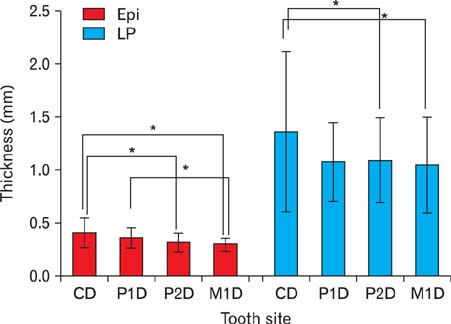
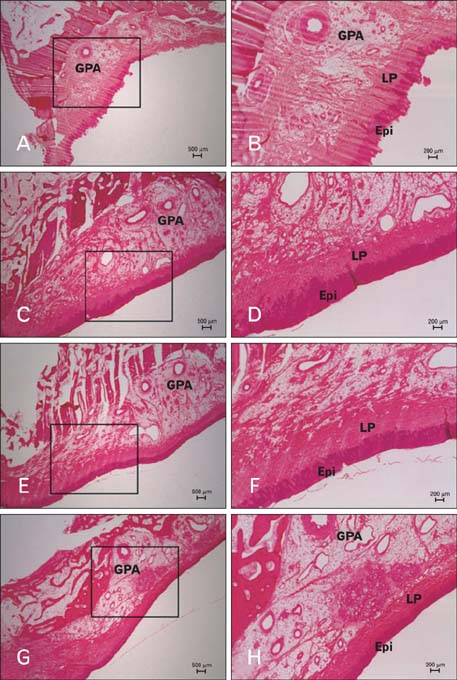
- This study aimed to measure the thickness of the epithelium and lamina propria of the palatal mucosa and to elucidate the location of the greater palatine artery to provide the anatomical basis for subepithelial connective tissue grafting. Thirty-two maxillary specimens, taken from the canine distal area to the first molar distal area, were embedded in paraffin and stained with hematoxylin-eosin. The thickness of the epithelium and lamina propria of the palatal mucosa was measured at three positions on these specimens, starting from 3 mm below the alveolar crest and in 3-mm intervals. The location of the greater palatine artery was evaluated by using image-processing software. The mean epithelial thickness decreased significantly in the posterior teeth; it was 0.41, 0.36, 0.32, and 0.30 mm in the canine, first premolar, second premolar, and first molar distal areas, respectively. The lamina propria was significantly thicker in the canine distal; it was 1.36, 1.08, 1.09, and 1.05 mm, respectively. The mean length from the alveolar crest to the greater palatine artery increased toward the posterior molar; it was 7.76, 9.21, 10.93, and 11.28 mm, respectively. The mean depth from the surface of the palatal mucosa to the greater palatine artery decreased from the canine distal to the first premolar distal but increased again toward the posterior molar; it was 3.97, 3.09, 3.58, and 5.50 mm, respectively. Detailed histological assessments of the lamina propria of the palatal mucosa and the greater palatine artery are expected to provide useful anatomical guidelines for subepithelial connective tissue grafting.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of 2 techniques of epithelial removal in subepithelial connective tissue graft surgery: a comparative histological study
Paola Marques de Mattos, Vula Papalexiou, Vinícius Augusto Tramontina, Sung Hyun Kim, Sônia Mara Luczyszyn, Patrícia Vida Cassi Bettega, Aline Cristina Batista Rodrigues Johann
J Periodontal Implant Sci. 2020;50(1):2-13. doi: 10.5051/jpis.2020.50.1.2.
Reference
-
1. Byun HY, Oh TJ, Abuhussein HM, Yamashita J, Soehren SE, Wang HL. Significance of the epithelial collar on the subepithelial connective tissue graft. J Periodontol. 2009; 80:924–932.2. Sedon CL, Breault LG, Covington LL, Bishop BG. The subepithelial connective tissue graft: part II. Histologic healing and clinical root coverage. J Contemp Dent Pract. 2005; 6:139–150.3. Langer L, Langer B. The subepithelial connective tissue graft for treatment of gingival recession. Dent Clin North Am. 1993; 37:243–264.4. Nanci A. Ten cate's oral histology: development, structure, and function. 6th ed. Seoul: Daehan Publishing Co.;2005. p. 333–376.5. McMinn RH. Last's anatomy regional and applied. 8th ed. Oxford: Churchill Livingstone;1990. p. 470–480.6. Li KK, Meara JG, Alexander A Jr. Location of the descending palatine artery in relation to the Le Fort I osteotomy. J Oral Maxillofac Surg. 1996; 54:822–825.7. Jeyaseelan N, Gupta M. Canals for the greater palatine nerve and vessels in the hard palate. J Anat. 1988; 156:231–233.8. Benninger B, Andrews K, Carter W. Clinical measurements of hard palate and implications for subepithelial connective tissue grafts with suggestions for palatal nomenclature. J Oral Maxillofac Surg. 2012; 70:149–153.9. Studer SP, Allen EP, Rees TC, Kouba A. The thickness of masticatory mucosa in the human hard palate and tuberosity as potential donor sites for ridge augmentation procedures. J Periodontol. 1997; 68:145–151.10. Müller HP, Schaller N, Eger T. Ultrasonic determination of thickness of masticatory mucosa: a methodologic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:248–253.11. Song JE, Um YJ, Kim CS, Choi SH, Cho KS, Kim CK, Chai JK, Jung UW. Thickness of posterior palatal masticatory mucosa: the use of computerized tomography. J Periodontol. 2008; 79:406–412.12. Lee YJ, Kwon YH, Park JB, Herr Y, Shin SI, Heo SJ, Chung JH. Epithelial thickness of the palatal mucosa: a histomorphometric study in Koreans. Anat Rec (Hoboken). 2010; 293:1966–1970.13. Prestin S, Rothschild SI, Betz CS, Kraft M. Measurement of epithelial thickness within the oral cavity using optical coherence tomography. Head Neck. 2012; 34:1777–1781.14. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985; 56:715–720.15. Mormann W, Schaer F, Firestone AR. The relationship between success of free gingival grafts and transplant thickness: revascularization and shrinkage: a one year clinical study. J Periodontol. 1981; 52:74–80.16. Kim JW, Kikkawa DO, Lemke BN. Donor site complications of hard palate mucosal grafting. Ophthal Plast Reconstr Surg. 1997; 13:36–39.17. Harris RJ. Formation of a cyst-like area after a connective tissue graft for root coverage. J Periodontol. 2002; 73:340–345.18. Parashis AO, Tatakis DN. Subepithelial connective tissue graft for root coverage: a case report of an unusual late complication of epithelial origin. J Periodontol. 2007; 78:2051–2056.19. Kolliyavar B, Setty S, Thakur SL. Determination of thickness of palatal mucosa. J Indian Soc Periodontol. 2012; 16:80–83.20. Johnson RE, Sigman JD, Funk GF, Robinson RA, Hoffman HT. Quantification of surgical margin shrinkage in the oral cavity. Head Neck. 1997; 19:281–286.21. Reiser GM, Bruno JF, Mahan PE, Larkin LH. The subepithelial connective tissue graft palatal donor site: anatomic considerations for surgeons. Int J Periodontics Restorative Dent. 1996; 16:130–137.22. Wara-aswapati N, Pitiphat W, Chandrapho N, Rattanayatikul C, Karimbux N. Thickness of palatal masticatory mucosa associated with age. J Periodontol. 2001; 72:1407–1412.23. Won SY, Kim DH, Yang HM, Park JT, Kwak HH, Hu KS, Kim HJ. Clinical and anatomical approach using Sihler's staining technique (whole mount nerve stain). Anat Cell Biol. 2011; 44:1–7.24. Fu JH, Hasso DG, Yeh CY, Leong DJ, Chan HL, Wang HL. The accuracy of identifying the greater palatine neurovascular bundle: a cadaver study. J Periodontol. 2011; 82:1000–1006.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of palatal defect using palatal flap
- The thickness of palatal masticatory mucosa
- Laterally positioned flap using subepithelial connective tissue graft for iatrogenic gingival recession treatment
- Morphological Investigations on the Epithelium and Subepithelial Connective Tissue of the Human Paranasal Sinus Mucosa
- Simultaneous Hard Tissue and Soft Tissue Graft with Dental Implant Placement and Provisionalization: A Case Report