Allergy Asthma Immunol Res.
2013 Mar;5(2):88-95. 10.4168/aair.2013.5.2.88.
Clinical Predictors of Primary Immunodeficiency Diseases in Children
- Affiliations
-
- 1Department of Pediatric Allergy and Immunology, Children's Hospital, Faculty of Medicine, Ain Shams University, Cairo, Egypt. shereen.m.reda@gmail.com
- 2Department of Clinical Pathology, Faculty of Medicine, Ain Shams University, Cairo, Egypt.
- KMID: 2260343
- DOI: http://doi.org/10.4168/aair.2013.5.2.88
Abstract
- PURPOSE
To promote awareness of primary immunodeficiency (PID), the "10 warning signs" of PID and an immunodeficiency-related (IDR) score were developed. However, their efficiency in identifying PID cases was not sufficiently evaluated in clinical practice. The objective of this study was to test the validity of the 10 warning signs and IDR score in identifying PID among children with recurrent infections at a tertiary pediatric hospital in Egypt.
METHODS
A retrospective analysis of the medical records of 204 patients was performed. Of these patients, 92 had defined PID diseases and 112 were considered non-PID cases because investigations were inconclusive.
RESULTS
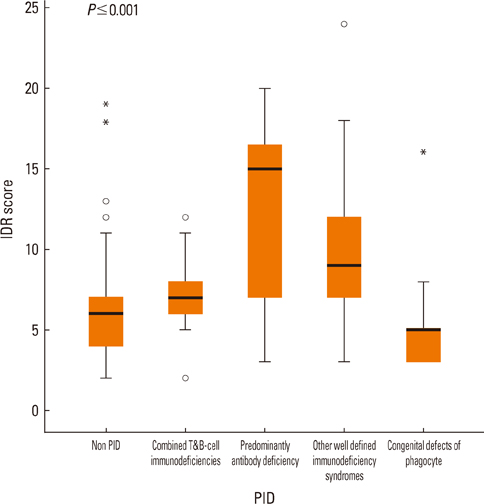
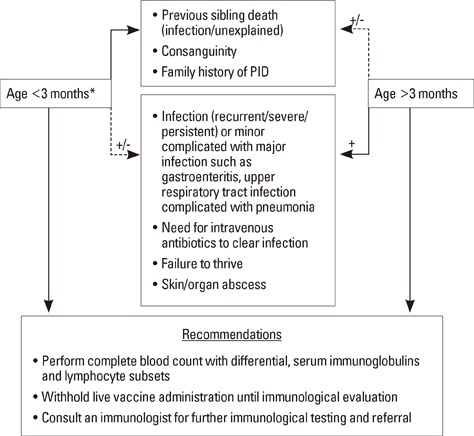
Demonstrating two warning signs and an IDR score of 6 led to sensitivities of 94 and 66%, respectively, and specificities of 64 and 75%, respectively, in identifying PID cases. The strongest predictor of PID was family history that, if combined with the need for intravenous antibiotics, recurrent deep-seated infections, and failure to thrive, could identify 81% of PID patients. A family history of PID, sibling death, and/or parental consanguinity would predict 92% of combined immunodeficiencies, 92% of phagocyte defects, 87% of well-identified immunodeficiency syndromes, and 84% of antibody deficiency if the need for intravenous antibiotics is considered in the latter.
CONCLUSIONS
The 10 warning signs and IDR score do not aid in an early diagnosis of severe PID. Educational campaigns should target pediatricians aiming to increase PID awareness and to address family history of PID, parental consanguinity, and previous sibling death as key predictors of PID in communities with a high prevalence of consanguineous marriages.
Keyword
MeSH Terms
Figure
Reference
-
1. Conley ME, Notarangelo LD, Etzioni A. Diagnostic criteria for primary immunodeficiencies. Representing PAGID (Pan-American Group for Immunodeficiency) and ESID (European Society for Immunodeficiencies). Clin Immunol. 1999. 93:190–197.2. Boyle JM, Buckley RH. Population prevalence of diagnosed primary immunodeficiency diseases in the United States. J Clin Immunol. 2007. 27:497–502.3. Bonilla FA, Geha RS. 12. Primary immunodeficiency diseases. J Allergy Clin Immunol. 2003. 111:S571–S581.4. Woroniecka M, Ballow M. Office evaluation of children with recurrent infection. Pediatr Clin North Am. 2000. 47:1211–1224.5. de Vries E. Clinical Working Party of the European Society for Immunodeficiencies (ESID). Patient-centred screening for primary immunodeficiency: a multi-stage diagnostic protocol designed for non-immunologists. Clin Exp Immunol. 2006. 145:204–214.6. Sewell WA, Khan S, Doré PC. Early indicators of immunodeficiency in adults and children: protocols for screening for primary immunological defects. Clin Exp Immunol. 2006. 145:201–203.7. Champi C. Primary immunodeficiency disorders in children: prompt diagnosis can lead to lifesaving treatment. J Pediatr Health Care. 2002. 16:16–21.8. Bonilla FA, Bernstein IL, Khan DA, Ballas ZK, Chinen J, Frank MM, Kobrynski LJ, Levinson AI, Mazer B, Nelson RP Jr, Orange JS, Routes JM, Shearer WT, Sorensen RU. American Academy of Allergy, Asthma and Immunology. American College of Allergy, Asthma and Immunology. Joint Council of Allergy, Asthma and Immunology. Practice parameter for the diagnosis and management of primary immunodeficiency. Ann Allergy Asthma Immunol. 2005. 94:S1–63.9. National Primary Immunodeficiency Resource Center [Internet]. cited 2010 Oct 17. Available from: http://www.info4pi.org.10. Cunningham-Rundles C, Sidi P, Estrella L, Doucette J. Identifying undiagnosed primary immunodeficiency diseases in minority subjects by using computer sorting of diagnosis codes. J Allergy Clin Immunol. 2004. 113:747–755.11. Yarmohammadi H, Estrella L, Doucette J, Cunningham-Rundles C. Recognizing primary immune deficiency in clinical practice. Clin Vaccine Immunol. 2006. 13:329–332.12. World Health Organization. Global Health Observatory (GHO): Egypt Health Profile [Internet]. cited 2011 Dec 20. Available from: http://www.who.int/gho/countries/egy/country_profiles/en/index.html.13. European Society for Immunodeficiency (ESID) [Internet]. cited 2011 Dec 14. Available from: http://www.esid.org/registry-number-of-patients.14. Reda SM, Afifi HM, Amine MM. Primary immunodeficiency diseases in Egyptian children: a single-center study. J Clin Immunol. 2009. 29:343–351.15. Primary immunodeficiency diseases. Report of a WHO scientific group. Clin Exp Immunol. 1997. 109:Suppl 1. 1–28.16. International Union of Immunological Societies Expert Committee on Primary Immunodeficiencies. Notarangelo LD, Fischer A, Geha RS, Casanova JL, Chapel H, Conley ME, Cunningham-Rundles C, Etzioni A, Hammartröm L, Nonoyama S, Ochs HD, Puck J, Roifman C, Seger R, Wedgwood J. Primary immunodeficiencies: 2009 update. J Allergy Clin Immunol. 2009. 124:1161–1178.17. Subbarayan A, Colarusso G, Hughes SM, Gennery AR, Slatter M, Cant AJ, Arkwright PD. Clinical features that identify children with primary immunodeficiency diseases. Pediatrics. 2011. 127:810–816.18. Enriquez L, Gómez G, Rodriguez V, Patiño P, Orrego J, Franco J. F.87. Screening of patients suspected of having a primary immunodeficiency disorder: Statistical performance of criteria employed for their initial identification. Clin Immunol. 2008. 127:Suppl. S71–S72.19. Moin M, Aghamohammadi A, Kouhi A, Tavassoli S, Rezaei N, Ghaffari SR, Gharagozlou M, Movahedi M, Purpak Z, Mirsaeid Ghazi B, Mahmoudi M, Farhoudi A. Ataxia-telangiectasia in Iran: clinical and laboratory features of 104 patients. Pediatr Neurol. 2007. 37:21–28.20. Al-Herz W. Primary immunodeficiency disorders in Kuwait: first report from Kuwait National Primary Immunodeficiency Registry (2004--2006). J Clin Immunol. 2008. 28:186–193.21. Barbouche MR, Galal N, Ben-Mustapha I, Jeddane L, Mellouli F, Ailal F, Bejaoui M, Boutros J, Marsafy A, Bousfiha AA. Primary immunodeficiencies in highly consanguineous North African populations. Ann N Y Acad Sci. 2011. 1238:42–52.22. Brown L, Xu-Bayford J, Allwood Z, Slatter M, Cant A, Davies EG, Veys P, Gennery AR, Gaspar HB. Neonatal diagnosis of severe combined immunodeficiency leads to significantly improved survival outcome: the case for newborn screening. Blood. 2011. 117:3243–3246.23. Yilmaz-Demirdag Y. Should newborns be screened for immunodeficiency?: lessons learned from infants with recurrent otitis media. Curr Allergy Asthma Rep. 2011. 11:491–498.24. MacGinnitie A, Aloi F, Mishra S. Clinical characteristics of pediatric patients evaluated for primary immunodeficiency. Pediatr Allergy Immunol. 2011. 22:671–675.25. Arkwright PD, Gennery AR. Ten warning signs of primary immunodeficiency: a new paradigm is needed for the 21st century. Ann N Y Acad Sci. 2011. 1238:7–14.26. Modell V, Gee B, Lewis DB, Orange JS, Roifman CM, Routes JM, Sorensen RU, Notarangelo LD, Modell F. Global study of primary immunodeficiency diseases (PI)--diagnosis, treatment, and economic impact: an updated report from the Jeffrey Modell Foundation. Immunol Res. 2011. 51:61–70.27. Hossny E, El-Awady H, El-Feky M, El-Owaidy R. Screening for B- and T-cell defects in Egyptian infants and children with suspected primary immunodeficiency. Med Sci Monit. 2009. 15:CR217–CR225.28. de Vries E. European Society for Immunodeficiencies (ESID) members. Patient-centred screening for primary immunodeficiency, a multi-stage diagnostic protocol designed for non-immunologists: 2011 update. Clin Exp Immunol. 2012. 167:108–119.29. van der Burg M, van Zelm MC, van Dongen JJ. Molecular diagnostics of primary immunodeficiencies: benefits and future challenges. Adv Exp Med Biol. 2009. 634:231–241.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection and Diagnosis of Primary Immunodeficiency Diseases
- Usefulness of Lymphocyte Subset Analysis Using Primary Immunodeficiency Orientation Tube Panel: Two Cases with Primary Immunodeficiency Diseases
- Clinical Features of Primary Immunodeficiency Diseases
- Pulmonary Complications in Primary Immunodeficiency Diseases
- A Case of Ankylosing Spondylitis in a Patient with Human Immunodeficiency Virus