Korean J Hematol.
2009 Sep;44(3):148-152. 10.5045/kjh.2009.44.3.148.
A Case of Acute Myeloid Leukemia with Mediastinal Sarcoma
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University, College of Medicine, Busan, Korea. kimhj@dau.ac.kr
- 2Department of Laboratory Medicine, Dong-A University, College of Medicine, Busan, Korea.
- 3Department of Pathology, Dong-A University, College of Medicine, Busan, Korea.
- KMID: 2252133
- DOI: http://doi.org/10.5045/kjh.2009.44.3.148
Abstract
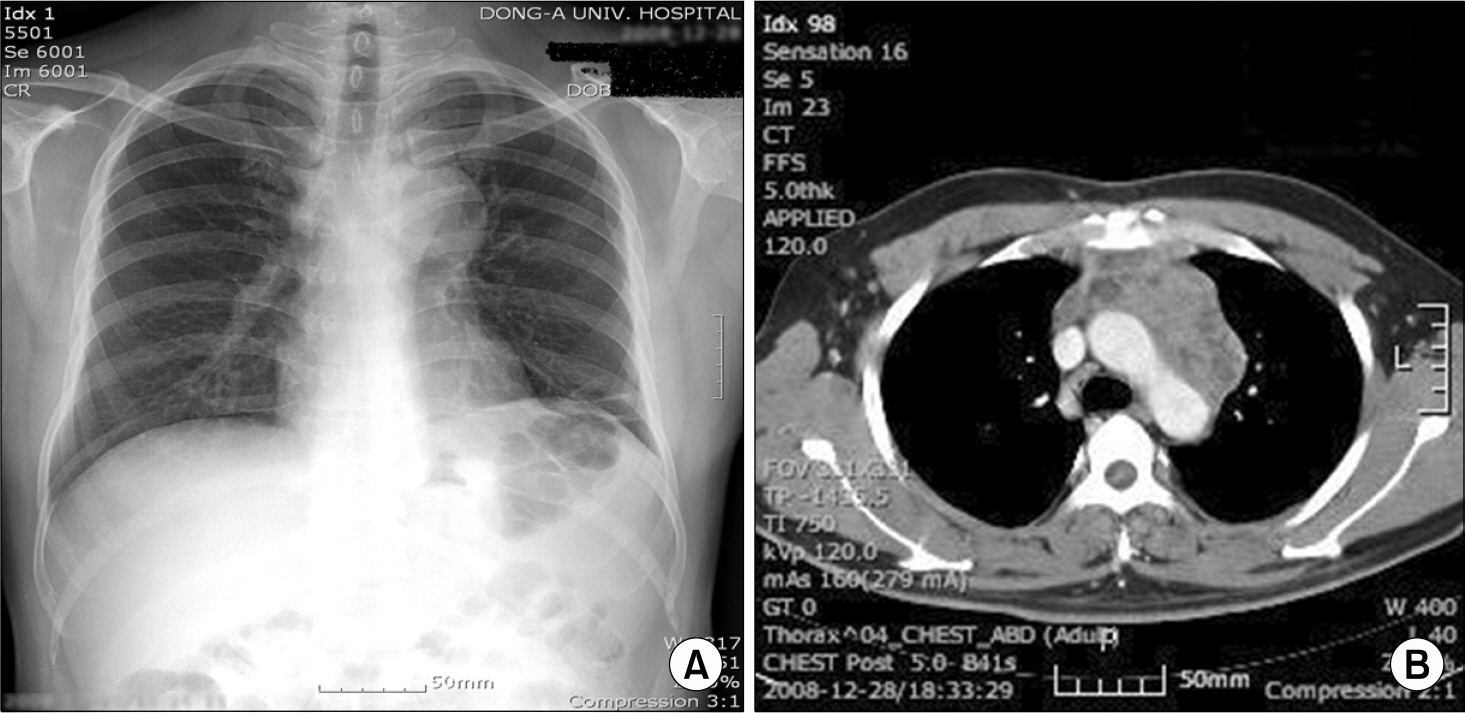
- Myeloid sarcoma (MS) is a solid extramedullary tumor that is composed of immature myeloid cells. The incidence of MS in patients with acute myeloid leukemia (AML) has been reported to be 3~8%. Lymph nodes are the most frequent site of presentation for MS, and other clinical presentations such as an abdominal mass with bowel involvement, a pancreatic mass, isolated central nervous system infiltration, a testicular mass and breast lumps have also been reported. AML with mediastinal MS is a relatively rare disease. The patients with AML with mediastinal MS has been reported to have complex cytogenetic abnormalities and a poor long-term prognosis. The optimal treatment of AML with MS remains to be determined. We report here on an unusual case of a 37-year-old man who presented multiple lymph node enlargements on the neck and a huge mediastinal mass that was considered to be lymphoma. He was finally diagnosed as AML with MS according to the surgical excisional biopsy of a left supraclavicular lymph node and bone marrow examination. He achieved complete remission and the multiple enlarged lymph nodes on the neck and the mediastinal mass disappeared after remission induction chemotherapy. Thereafter, he received HLA-matched unrelated allogenic hematopoietic stem cell transplantation.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Brunning RD, Matutes E, Flandrin G, et al. Acute myeloid leukemia not otherwise categorised. In: Jaffe ES, Harris NL, Stein H, Vardiman JW, eds. World Health Organization classification of tumours, pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon, France: IARC Press. 2001. 104–5.2. Meis JM, Butler JJ, Osborne BM, Manning JT. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986; 58:2697–709.
Article3. Muss HB, Moloney WC. Chloroma and other myeloblastic tumors. Blood. 1973; 42:721–8.
Article4. Paydas S, Zorludemir S, Ergin M. Granulocytic sarcoma: 32 cases and review of the literature. Leuk Lymphoma. 2006; 47:2527–41.
Article5. Byrd JC, Edenfield WJ, Shields DJ, Dawson NA. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: a clinical review. J Clin Oncol. 1995; 13:1800–16.
Article6. Harris NL, Jaffe ES, Diebold J, et al. World health organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the clinical advisory committee meeting-airlie house, virginia, november 1997. J Clin Oncol. 1999; 17:3835–49.
Article7. Ramasamy K, Lim Z, Pagliuca A, Devereux S, Ho AY, Mufti GJ. Acute myeloid leukaemia presenting with mediastinal myeloid sarcoma: report of three cases and review of literature. Leuk Lymphoma. 2007; 48:290–4.
Article8. Takasugi JE, Godwin JD, Marglin SI, Petersdorf SH. Intrathoracic granulocytic sarcomas. J Thorac Imaging. 1996; 11:223–30.
Article9. Bae HS, Chung NS, Park PW, et al. Report of 8 case of granulocytic sarcoma. Korean J Hematol. 1982; 17:175–83.10. Menasce LP, Banerjee SS, Beckett E, Harris M. Extramedullary myeloid tumour (granulocytic sarcoma) is often misdiagnosed: a study of 26 cases. Histopathology. 1999; 34:391–8.
Article11. Finnegan DP, Jones FG, McMullin MF. Acute myeloid leukemia with concurrent myeloid sarcoma treated with autologous bone marrow transplantation: two illustrative cases and a literature review. Hematol Oncol. 2005; 23:133–5.
Article12. Breccia M, Mandelli F, Petti MC, et al. Clinicopathological characteristics of myeloid sarcoma at diagnosis and during follow-up: report of 12 cases from a single institution. Leuk Res. 2004; 28:1165–9.
Article13. Yamauchi K, Yasuda M. Comparison in treatments of nonleukemic granulocytic sarcoma: report of two cases and a review of 72 cases in the literature. Cancer. 2002; 94:1739–46.14. Takada S, Ito K, Sakura T, et al. Three AML patients with existing or pre-existing intracerebral granulocytic sarcomas who were successfully treated with allogeneic bone marrow transplantations. Bone Marrow Transplant. 1999; 23:731–4.
Article15. Kowal-Vern A, Johnson FL, Trujillo Y, et al. Granulocytic sarcoma of the ileum treated by bone marrow transplantation. Am J Pediatr Hematol Oncol. 1991; 13:34–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraparenchymal Myeloid Sarcoma and Subsequent Spinal Myeloid Sarcoma for Acute Myeloblastic Leukemia
- Myeloid Sarcoma of Peritoneum in Acute Myeloid Leukemia Patient with Inversion of Chromosome 16
- A Case of Myeloid Sarcoma Preceding the Diagnosis of Acute Myeloid Leukemia
- A Case of Temporal Bone Myeloid Sarcoma
- Granulocytic Sarcoma in the Leg Mimicking Hemorrhagic Abscess