J Gynecol Oncol.
2012 Jul;23(3):159-167. 10.3802/jgo.2012.23.3.159.
Radiation therapy with chemotherapy for patients with cervical cancer and supraclavicular lymph node involvement
- Affiliations
-
- 1Department of Radiation Oncology, Gachon Gil Medical Center, Incheon, Korea. kyu22@gilhospital.com
- 2Department of Obstetrics and Gynecology, Gachon Gil Medical Center, Incheon, Korea.
- 3Department of Internal Medicine, Gachon Gil Medical Center, Incheon, Korea.
- 4Department of Biochemistry and Molecular Biology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2245174
- DOI: http://doi.org/10.3802/jgo.2012.23.3.159
Abstract
OBJECTIVE
We wanted to evaluate the outcomes of cervical cancer patients with supraclavicular lymph node (SCLN) involvement and who received radiation therapy (RT) combined with chemotherapy.
METHODS
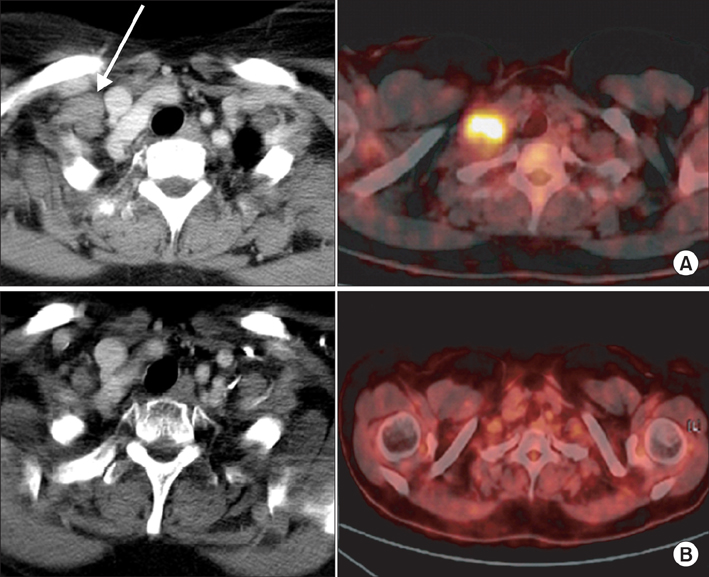
From August 2001 to April 2009, nine cervical cancer patients with SCLN involvement were treated by RT and cisplatin-based chemotherapy. Most of the patients (8/9, 88.9%) also had a positive para-aortic lymph node (PALN). The RT field was designed to include the whole pelvis, the involved PALNs and the SCLN area. The median SCLN RT dose was 66.6 Gy (range, 60 to 70 Gy).
RESULTS
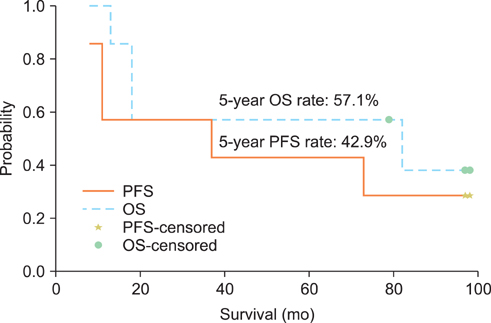
The median follow-up period was 61 months (range, 13 to 98 months). The 3- and 5-year overall survival rates were 66.7% and 55.6%, respectively and the 3- and 5-year progression-free survival rates were 66.7% and 44.4%, respectively. The acute hematologic toxicities according to the criteria of Radiation Therapy of Oncology Group (RTOG) were G1/2 leucopenia in 3 (33.3%), G3/4 leukopenia in 6 (66.7%), G1/2 anemia in 7 (77.8%), G3 anemia in 1 (11.1%), G2 thrombocytopenia in 2 (22.2%), and G3/4 thrombocytopenia in 2 (22.2%). Within 6 months after RT, most of the patients (5/6, 83.3%) recovered from the G3/4 leukopenia, except for 1 patient who received chemotherapy after completing RT due to subsequent bone metastasis.
CONCLUSION
For patients with advanced cervix cancer and SCLN involvement, RT with chemotherapy as active therapy can be expected to provide favorable results, although there is an increased risk of G3/4 hematologic toxicity.
MeSH Terms
Figure
Cited by 1 articles
-
Impact of Chemoradiation on Prognosis in Stage IVB Cervical Cancer with Distant Lymphatic Metastasis
Hee Seung Kim, Taehun Kim, Eung Seok Lee, Hak Jae Kim, Hyun Hoon Chung, Jae Weon Kim, Yong Sang Song, Noh Hyun Park
Cancer Res Treat. 2013;45(3):193-201. doi: 10.4143/crt.2013.45.3.193.
Reference
-
1. Perez CA, Camel HM, Kuske RR, Kao MS, Galakatos A, Hederman MA, et al. Radiation therapy alone in the treatment of carcinoma of the uterine cervix: a 20-year experience. Gynecol Oncol. 1986. 23:127–140.2. Eifel PJ, Winter K, Morris M, Levenback C, Grigsby PW, Cooper J, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of Radiation Therapy Oncology Group trial (RTOG) 90-01. J Clin Oncol. 2004. 22:872–880.3. Kim K, Cho SY, Kim BJ, Kim MH, Choi SC, Ryu SY. The type of metastasis is a prognostic factor in disseminated cervical cancer. J Gynecol Oncol. 2010. 21:186–190.4. Yao ZH, Wu AR. Supraclavicular lymph node metastasis from carcinoma of the uterine cervix after radiotherapy - analysis of 219 patients. Zhonghua Zhong Liu Za Zhi. 1988. 10:230–232.5. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981. 47:207–214.6. Pecorelli S, Zigliani L, Odicino F. Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet. 2009. 105:107–108.7. Qiu JT, Ho KC, Lai CH, Yen TC, Huang YT, Chao A, et al. Supraclavicular lymph node metastases in cervical cancer. Eur J Gynaecol Oncol. 2007. 28:33–38.8. Tran BN, Grigsby PW, Dehdashti F, Herzog TJ, Siegel BA. Occult supraclavicular lymph node metastasis identified by FDG-PET in patients with carcinoma of the uterine cervix. Gynecol Oncol. 2003. 90:572–576.9. Chao A, Ho KC, Wang CC, Cheng HH, Lin G, Yen TC, et al. Positron emission tomography in evaluating the feasibility of curative intent in cervical cancer patients with limited distant lymph node metastases. Gynecol Oncol. 2008. 110:172–178.10. Hong JH, Tsai CS, Lai CH, Chang TC, Wang CC, Chou HH, et al. Recurrent squamous cell carcinoma of cervix after definitive radiotherapy. Int J Radiat Oncol Biol Phys. 2004. 60:249–257.11. Stehman FB, Bundy BN, Hanjani P, Fowler WC, Abdulhay G, Whitney CW. Biopsy of the scalene fat pad in carcinoma of the cervix uteri metastatic to the periaortic lymph nodes. Surg Gynecol Obstet. 1987. 165:503–506.12. Beyer FD Jr, Murphy A. Patterns of spread of invasive cancer of the uterine cervix. Cancer. 1965. 18:34–40.13. Shin JW, Lee KC, Lee SH, Choi JH, Lee KB, Park CY. Concurrent chemoradiation therapy in cervical cancer with para-aortic lymph node involvement. Korean J Gynecol Oncol. 2007. 18:108–113.14. Grigsby PW, Perez CA, Chao KS, Herzog T, Mutch DG, Rader J. Radiation therapy for carcinoma of the cervix with biopsy-proven positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2001. 49:733–738.15. Kim YS, Kim JH, Ahn SD, Lee SW, Shin SS, Nam JH, et al. High-dose extended-field irradiation and high-dose-rate brachytherapy with concurrent chemotherapy for cervical cancer with positive para-aortic lymph nodes. Int J Radiat Oncol Biol Phys. 2009. 74:1522–1528.16. Portelance L, Chao KS, Grigsby PW, Bennet H, Low D. Intensity-modulated radiation therapy (IMRT) reduces small bowel, rectum, and bladder doses in patients with cervical cancer receiving pelvic and para-aortic irradiation. Int J Radiat Oncol Biol Phys. 2001. 51:261–266.17. Ahmed RS, Kim RY, Duan J, Meleth S, De Los Santos JF, Fiveash JB, et al. IMRT dose escalation for positive para-aortic lymph nodes in patients with locally advanced cervical cancer while reducing dose to bone marrow and other organs at risk. Int J Radiat Oncol Biol Phys. 2004. 60:505–512.18. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999. 340:1154–1161.19. Sood BM, Gorla GR, Garg M, Anderson PS, Fields AL, Runowicz CD, et al. Extended-field radiotherapy and high-dose-rate brachytherapy in carcinoma of the uterine cervix: clinical experience with and without concomitant chemotherapy. Cancer. 2003. 97:1781–1788.20. Kim JS, Kim JS, Kim SY, Kim KH, Cho MJ. Hyperfractionated radiotherapy with concurrent chemotherapy for para-aortic lymph node recurrence in carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2003. 55:1247–1253.21. Grigsby PW, Lu JD, Mutch DG, Kim RY, Eifel PJ. Twice-daily fractionation of external irradiation with brachytherapy and chemotherapy in carcinoma of the cervix with positive para-aortic lymph nodes: phase II study of the Radiation Therapy Oncology Group 92-10. Int J Radiat Oncol Biol Phys. 1998. 41:817–822.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Journal correction: Radiation therapy with chemotherapy for patients with cervical cancer and supraclavicular lymph node involvement
- Concurrent chemoradiation therapy in cervical cancer with para-aortic lymph node involvement
- Supraclavicular Lymph Node Excision Biopsy in Patients with Suspected Supraclavicular Lymph Node Metastasis of Lung Cancer: Experience in a Tertiary Hospital
- Combined Multimodality Treatment including Surgery
- Prognosis of the Patients Showing Metastasis to the Para-aortic or/and Supraclavicular Lymph Nodes at the Time of Diagnosis of Recurrence of the Cervical Cancer