Korean J Hepatobiliary Pancreat Surg.
2013 Feb;17(1):34-37. 10.14701/kjhbps.2013.17.1.34.
Primary hepatic neuroendocrine carcinoma
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jw.joh@samsung.com
- 2Division of Gastroenterology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2243166
- DOI: http://doi.org/10.14701/kjhbps.2013.17.1.34
Abstract
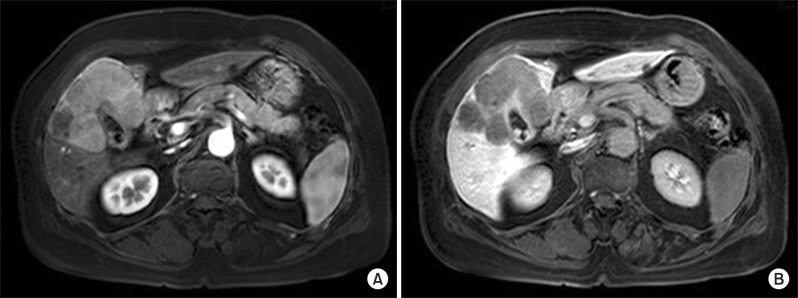
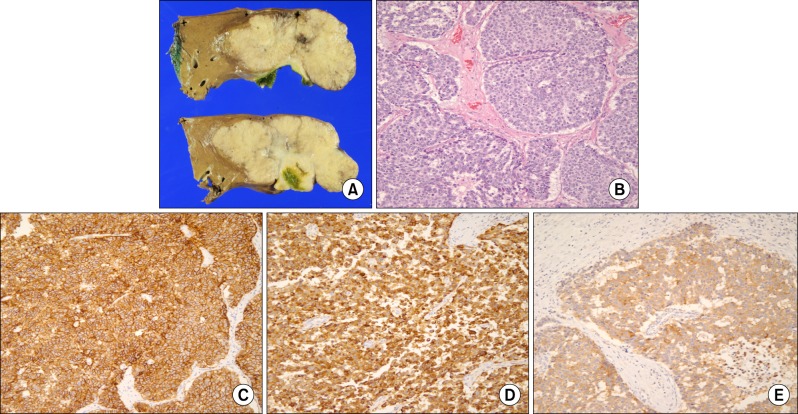
- A 67-year-old woman was admitted to our hospital under suspicion of a hepatic tumor, which had been previously diagnosed to be an adenocarcinoma by fine needle aspiration. Computed tomography and magnetic resonance imaging revealed a large tumor measuring 9 cm in diameter in Couinaud's hepatic segments 4, 5, and 8. We diagnosed the patient to have primary liver cancer, and suspected intrahepatic cholangiocarcinoma preoperatively. We performed a central hepatectomy. According to the immunohistochemical findings of the resected specimen, the tumor was diagnosed to be a primary neuroendocrine carcinoma in the liver. The patient is presently alive without recurrence at 3 months after hepatic resection.
MeSH Terms
Figure
Cited by 1 articles
-
젊은 나이에 발생하는 원발성 간 신경내분비 종양 1예
Sanghwa Song, Yangseok Koh
Korean J Gastroenterol. 2022;79(1):35-40. doi: 10.4166/kjg.2021.139.
Reference
-
1. Gould VE, Jao W, Chejfec G, et al. Neuroendocrine carcinomas of the gastrointestinal tract. Semin Diagn Pathol. 1984; 1:13–18. PMID: 6400627.2. Knox CD, Anderson CD, Lamps LW, et al. Long-term survival after resection for primary hepatic carcinoid tumor. Ann Surg Oncol. 2003; 10:1171–1175. PMID: 14654473.
Article3. Mima K, Beppu T, Murata A, et al. Primary neuroendocrine tumor in the liver treated by hepatectomy: report of a case. Surg Today. 2011; 41:1655–1660. PMID: 21969201.
Article4. Pilichowska M, Kimura N, Ouchi A, et al. Primary hepatic carcinoid and neuroendocrine carcinoma: clinicopathological and immunohistochemical study of five cases. Pathol Int. 1999; 49:318–324. PMID: 10365851.
Article5. Ishida M, Seki K, Tatsuzawa A, et al. Primary hepatic neuroendocrine carcinoma coexisting with hepatocellular carcinoma in hepatitis C liver cirrhosis: report of a case. Surg Today. 2003; 33:214–218. PMID: 12658390.
Article6. Donadon M, Torzilli G, Palmisano A, et al. Liver resection for primary hepatic neuroendocrine tumours: report of three cases and review of the literature. Eur J Surg Oncol. 2006; 32:325–328. PMID: 16426802.
Article7. Huang YQ, Xu F, Yang JM, et al. Primary hepatic neuroendocrine carcinoma: clinical analysis of 11 cases. Hepatobiliary Pancreat Dis Int. 2010; 9:44–48. PMID: 20133228.8. Hendy GN, Bevan S, Mattei MG, et al. Chromogranin A. Clin Invest Med. 1995; 18:47–65. PMID: 7768066.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Gastric Neuroendocrine Tumor with Hepatic Metastasis
- Primary large cell neuroendocrine carcinoma of the common hepatic duct mimicking a Klatskin tumor
- Primary Neuroendocrine Carcinoma of the Breast: A Case Report and Literature Review
- Small-cell neuroendocrine carcinoma of the breast
- Gastroenteropancreatic Neuroendocrine Tumor with Hepatic Metastasis Misdiagnosed as Hepatocellular Carcinoma