Korean J Crit Care Med.
2015 Aug;30(3):227-230. 10.4266/kjccm.2015.30.3.227.
Unexpected Multiple Organ Infarctions in a Poisoned Patient
- Affiliations
-
- 1Department of Emergency Medicine, Pusan National University Hospital, Busan, Korea. 98hansoft@hanmail.net
- KMID: 2227655
- DOI: http://doi.org/10.4266/kjccm.2015.30.3.227
Abstract
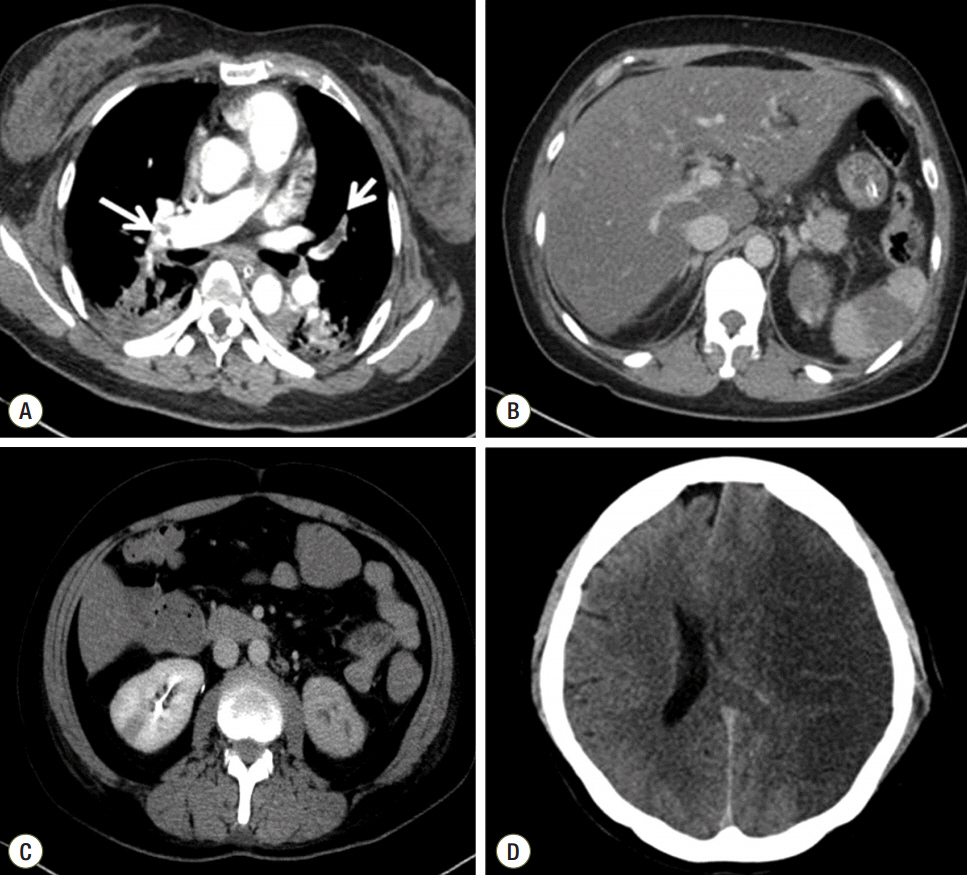
- Predisposing factors for venous thrombosis can be identified in the majority of patients with established venous thromboembolism (VTE). However, an obvious precipitant may not be identified during the initial evaluation of such patients. In the present case, a 47-year-old female presented to the emergency department of our hospital after ingesting multiple drugs. She had no VTE-related risk factors or previous episodes, nor any family history of VTE. After admission to the intensive care unit sudden hypoxemia developed, and during the evaluation cerebral, renal, and splenic infarctions with pulmonary embolisms were diagnosed. However, the sources of the emboli could not be identified by transthoracic echocardiography or computed tomography angiography. Protein C deficiency was identified several days later. We recommend that hypercoagulable states be taken into consideration, especially when unexplained thromboembolic events develop in multiple or unusual venous sites.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Lane DA, Mannucci PA, Bauer KA, Bertina RM, Bochkov NP, Boulyjenkov V, et al. Inherited thrombophilia: Part 1. Thromb Haemost. 1996; 76:651–62.
Article2. Bauer KA. The thrombophilias: well-defined risk factors with uncertain therapeutic implications. Ann Intern Med. 2001; 135:367–73.
Article3. Clouse LH, Comp PC. The regulation of hemostasis: the protein C system. N Engl J Med. 1996; 314:1298–304.
Article4. Tait RC, Walker ID, Reitsma PH, Islam SI, McCall F, Poort SR, et al. Prevalence of protein C deficiency in the healthy population. Thromb Haemost. 1995; 73:87–93.
Article5. Miletich J, Sherman L, Broze G Jr. Absence of thrombosis in subjects with heterozygous protein C deficiency. N Engl J Med. 1987; 317:991–6.
Article6. van der Meer FJ, Koster T, Vandenbroucke JP, Briët E, Rosendaal FR. The Leiden Thrombophilia Study (LETS). Thromb Haemost. 1997; 78:631–5.
Article7. Tiong IY, Alkotob ML, Ghaffari S. Protein C deficiency manifesting as an acute myocardial infarction and ischemic stroke. Heart. 2003; 89:E7.8. Kohler J, Kasper J, Witt I, von Reutern GM. Ischemic stroke due to protein C deficiency. Stroke. 1990; 21:1077–80.
Article9. Magbool S, Rastogi V, Seth A, Singh S, Kumar V, Mustaqueem A. Protein C deficiency presenting as pulmonary embolism and myocardial infarction in the same patient. Thromb J. 2013; 11:19.10. Mainwaring CJ, Makris M, Thomas WE, Hampton KK, Preston FE. Mesenteric infarction due to combined protein C deficiency and prothrombin 20210 defects. Postgrad Med J. 1999; 75:742–3.
Article11. D’Angelo A, Vigano-D’Angelo S, Esmon CT, Comp PC. Acquired deficiencies of protein S. Protein S activity during oral anticoagulation, in liver disease, and in disseminated intravascular coagulation. J Clin Invest. 1988; 81:1445–54.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Absence of the Left Atrial Appendage: An Unexpected and Incidental Anomaly in a Patient with Multiple Cerebellar Infarctions
- Case of Renal Microaneurysms and Multiple Renal Infarctions in a Patient with Systemic Lupus Erythematosus
- Calcineurin Inhibitor Induced Multiple Infarctions
- Multiple embolic infarctions and intracranial hemorrhage in a patient with gestational trophoblastic disease
- Multiple Cerebral Infarctions after Intravenous Vitamin K Injection in a Patient with Trauma