Korean Circ J.
2007 Jan;37(1):33-38. 10.4070/kcj.2007.37.1.33.
Re-endothelization and Inflammatory Reaction at Site of Overlapping Drug-Eluting Stents in a Porcine Coronary In-Stent Restenosis Model
- Affiliations
-
- 1Department of Internal Medicine, Cheju National University, Jeju, Korea.
- 2The Heart Center of Chonnam National University Hospital, Chonnam National University Research Institute of Medical Sciences, Gwangju, Korea. myungho@chollian.net
- KMID: 2227091
- DOI: http://doi.org/10.4070/kcj.2007.37.1.33
Abstract
-
BACKGROUND AND OBJECTIVES: This study was conducted to evaluate the inflammatory reaction at sites of overlapping stents in a porcine in-stent restenosis (ISR) model.
MATERIALS AND METHODS
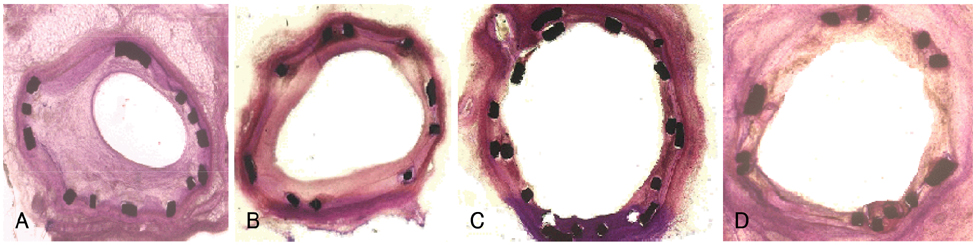
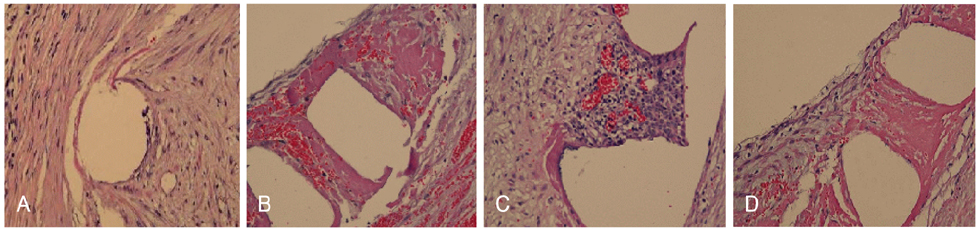
Twenty bare metal stents (BMS, Group I; n=10), 20 sirolimus-eluting stents (SES, Group II; n=10), 20 paclitaxel-eluting stents (PES, Group III; n=10), 10 PESs and 10 SESs (Group IV; n=10) were deployed and overlapped in the left anterior descending coronary arteries of 40 pigs. Follow-up coronary angiograms and histopathologic analysis were performed at 4 weeks after stenting.
RESULTS
The minimal luminal diameter of the overlapped segment at 4 weeks was smaller in group I than that in the other groups (1.78+/-0.13 mm vs. 2.79+/-0.09 mm vs. 2.90+/-0.04 mm vs. 2.80+/-0.07 mm, respectively, p<0.001). The neointimal area (5.51+/-0.58 mm2 vs. 2.38+/-0.53 mm2 vs. 2.07+/-0.37 mm2 vs. 2.39+/-0.58 mm2, respectively, p<0.001) and the area stenosis (68.74+/-4.02% vs. 27.79+/-4.73% vs. 23.66+/-3.24% vs. 27.63+/-4.07%, respectively, p<0.001) of the overlapped segment were significantly higher in Group I than that in the other groups. The inflammatory score of the overlapped segment was significantly higher in Group III than that in the other groups (1.80+/-0.42 vs. 2.10+/-0.32 vs. 2.90+/-0.31 vs. 2.50+/-0.52, respectively, p<0.001). The endothelization score of the overlapped segment was significantly lower in Group III than that in the other groups (2.80+/-0.42 vs. 2.30+/-0.67 vs. 1.30+/-0.48 vs. 2.10+/-0.74, respectively, p<0.001).
CONCLUSION
Compared with the BMS, the DES inhibits neointimal hyperplasia, but inflammation and poor endothelization are observed at the sites of overlapped stents.
Keyword
MeSH Terms
Figure
Reference
-
1. Serruys PW, Foley DP, Suttorp MJ, et al. A randomized comparison of the value of additional stenting after optimal balloon angioplasty for long coronary lesions: final results of the additional value of NIR stents for treatment of long coronary lesions (ADVANCE) study. J Am Coll Cardiol. 2002. 39:393–399.2. Kornowski R, Bhargava B, Fuchs S, et al. Procedural results and late clinical outcomes after percutaneous interventions using long (≥25 mm) versus short (<20 mm) stents. J Am Coll Cardiol. 2000. 35:612–618.3. Kornowski R, Mehran R, Satler LF, et al. Procedural results and late clinical outcomes following multivessel coronary stenting. J Am Coll Cardiol. 1999. 33:420–426.4. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005. 293:2126–2130.5. Kuchulakanti PK, Chu WW, Torguson R, et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation. 2006. 113:1108–1113.6. Finn AV, Kolodgie FD, Harnek J, et al. Differential response of delayed healing and persistent inflammation at sites of overlapping sirolimus- or paclitaxel-eluting stents. Circulation. 2005. 112:270–278.7. Ahn YK, Jeong MH, Kim JW, et al. Preventive effects of heparin coated stent on restenosis in the porcine model. Catheter Cardiovasc Interv. 1999. 48:324–330.8. Schwartz RS, Huber KC, Murphy JG, et al. Restenosis and the proportional neointimal response to coronary artery injury: results in a porcine model. J Am Coll Cardiol. 1992. 19:267–274.9. Schalij MJ, Udayachalerm W, Oemrawsingh P, Jukema JW, Reiber JH, Bruschke AV. Stenting of long coronary artery lesions: initial angiographic results and 6-month clinical outcome of the micro stent II-XL. Catheter Cardiovasc Interv. 1999. 48:105–112.10. Nebeker JR, Virmani R, Bennett CL, et al. Hypersensitivity cases associated with drug-eluting coronary stents: a review of available cases from the Research on Adverse Drug Events and Reports (RADAR) project. J Am Coll Cardiol. 2006. 47:175–181.11. Virmani R, Farb A, Guagliumi G, Kolodgie FD. Drug-eluting stents: caution and concerns for long-term outcome. Coron Artery Dis. 2004. 15:313–318.12. Azarbal B, Currier JW. Allergic reactions after the implantation of drug-eluting stents: is it the pill or the polymer? J Am Coll Cardiol. 2006. 47:182–183.13. Balakrishnan B, Tzafriri AR, Seifert P, Groothuis A, Rogers C, Edelman ER. Strut position, blood flow, and drug deposition: implications for single and overlapping drug-eluting stents. Circulation. 2005. 111:2958–2965.14. Babinska A, Markell MS, Salifu MO, Akoad M, Ehrlich YH, Kornecki E. Enhancement of human platelet aggregation and secretion induced by rapamycin. Nephrol Dial Transplant. 1998. 13:3153–3159.15. Stone GW, Ellis SG, Cox DA, et al. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent. Circulation. 2004. 109:1942–1947.16. Sousa JE, Costa MA, Sousa AG, et al. Two-year angiographic and intravascular ultrasound follow-up after implantation of sirolimus- eluting stents in human coronary arteries. Circulation. 2003. 107:381–383.17. Lemos PA, Serruys PW, van Domburg RT, et al. Unrestricted utilization of sirolimus-eluting stents compared with conventional bare stent implantation in the "real world". Circulation. 2004. 109:190–195.18. Karrillon GJ, Morice MC, Benveniste E, et al. Intracoronary stent implantation without ultrasound guidance and with replacement of conventional anticoagulation by antiplatelet therapy: 30-day clinical outcome of the French Multicenter Registry. Circulation. 1996. 94:1519–1527.19. Moussa I, di Mario C, Reimers B, Akiyama T, Tobis J, Colombo A. Subacute stent thrombosis in the era of intravascular ultrasound-guided coronary stenting without anticoagulation: frequency, predictors and clinical outcome. J Am Coll Cardiol. 1997. 29:6–12.20. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: a pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001. 103:1967–1971.21. Ong AT, McFadden EP, Regar E, de Jaegere PP, van Domburg RT, Serruys PW. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J Am Coll Cardiol. 2005. 45:2088–2092.22. McFadden EP, Stabile E, Regar E, et al. Late thrombosis in drugeluting coronary stents after discontinuation of antiplatelet therapy. Lancet. 2004. 364:1519–1521.23. Park HW, Jeong MH, Park OY, et al. The long-term clinical effects of heparin-coated coronary stent. Korean Circ J. 2002. 32:773–780.24. Kim W, Jeong MH, Cha KS, et al. The effect of anti-oxidants (carvedilol and probucol) loaded stents in a porcine coronary restenosis model. Circ J. 2005. 69:101–106.25. Kim W, Jeong MH, Hong YJ, et al. The long-term clinical results of a platelet glycoprotein IIb/IIIa receptor blocker (Abciximab: ReoPro®) coated stent in patients with acute myocardial infarction. Korean Circ J. 2004. 34:1063–1069.26. Hong YJ, Jeong MH, Kim W, et al. Effect of abciximab-coated stent on in-stent intimal hyperplasia in human coronary arteries. Am J Cardiol. 2004. 94:1050–1054.27. Park OY, Jeong MH, Kim JH, et al. The inhibitory effects of platelet glycoprotein IIb/IIIa receptor blocker-coated stent on neointima formation and inflammatory response in porcine coronary stent restenosis. Korean Circ J. 2003. 33:439–445.28. Lim SY, Jeong MH. Is heparin-coated stent effective in patients with acute myocardial infarction? Korean Circ J. 2004. 34:537–539.29. Kang WC, Han SH, Ahn TH, Son MS, Son JW, Shin EK. The long term clinical outcomes of primary PTCA with heparin coated stent in acute myocardial infarction. Korean Circ J. 2004. 34:540–547.30. Lim SY, Bae EH, Jeong MH, et al. The effect of oral administration of alpha lipoic acid and alpha lipoic acid coated stent in porcine in-stent restenosis model. Korean Circ J. 2006. 36:495–502.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug-Eluting Stent Strut Fracture as a Cause of Restenosis
- Systemic drug therapy and restenosis after drug-eluting stent implantation
- Coronary Restenosis after Drug-Eluting Stent Implantation in Diabetic Patients
- Drug-Eluting Stent Used to Treat a Case of Recurrent Right Coronary Artery In-Stent Restenoses often Accompanied by Acute Inferior Wall Myocardial Infarction
- Risk of Stent Stenosis after Implanting a First-Generation Drug-Eluting Stent and Drug Balloon Angioplasty