Korean Circ J.
2007 Oct;37(10):517-519. 10.4070/kcj.2007.37.10.517.
An Unusual Case of Exercise-Induced Idiopathic Brugada Electrocardiographic Pattern
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Kwandong University, Goyang, Korea. chodk123@paran.com
- 2Department of Pediatrics, College of Medicine, Kwandong University, Goyang, Korea.
- KMID: 2227054
- DOI: http://doi.org/10.4070/kcj.2007.37.10.517
Abstract
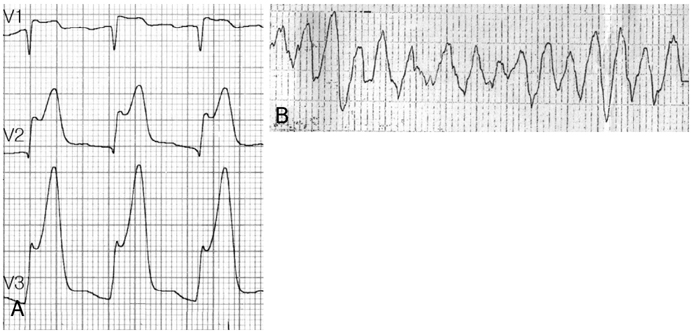
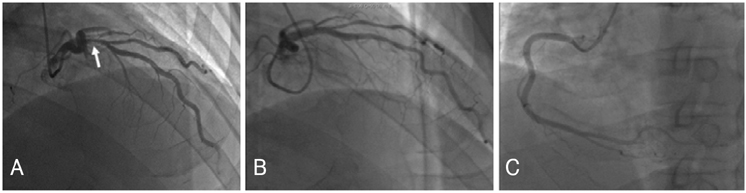
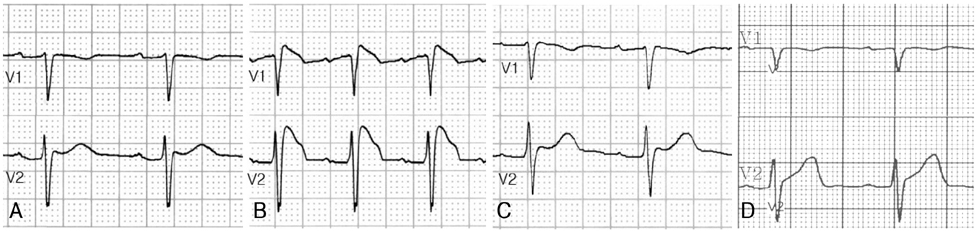
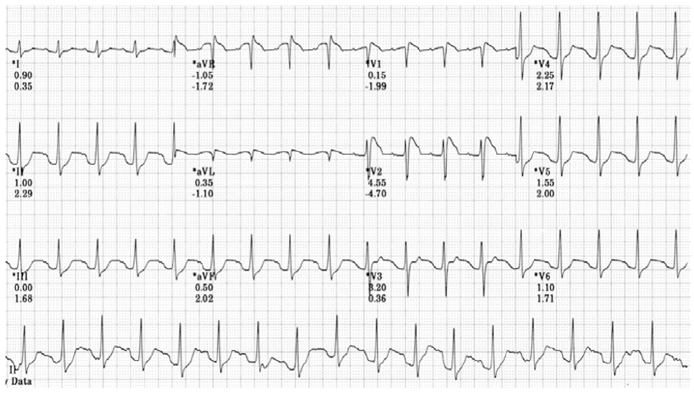
- An exercise-induced idiopathic Brugada electrocardiographic pattern during the effort phase is very rare. A 42-year-old male visited our cardiology clinic for chest discomfort. He has been treated for myocardial infarction 2 months ago. He underwent a treadmill test according to the Bruce protocol. Typical coved-type ST-segment elevation was found during the effort phase, and it gradually recovered after the exercise. The ST-segment elevation appeared to be unrelated to hypervagotonia. This elevation was not induced by a pharmacological test with flecainide. A significant ventricular arrhythmia was not induced by programmed ventricular stimulation. Hence, we discharged the patient without implantation of an implantable cardioverter defibrillator.
Keyword
MeSH Terms
Figure
Reference
-
1. Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome. Circulation. 2002. 106:2514–2519.2. Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for dudden death in patients without demonstrable structural heart disease. Circulation. 1998. 97:457–460.3. Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial ST-segment elevation, and sudden death in young people. Circulation. 2001. 103:710–717.4. Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003. 108:3092–3096.5. Brugada R, Brugada P, Brugada J. Electrocardiogram interpretation and class I blocker challenge in Brugada syndrome. J Electrocardiol. 2006. 39:Suppl. S115–S118.6. Mizumaki K, Fujiki A, Tsuneda T, et al. Vagal activity modulates spontaneous augmentation of ST elevation in the daily life of patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2004. 15:667–673.7. Brugada R, Brugada J, Antzelevitch C, et al. Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts. Circulation. 2000. 101:510–515.8. Brugada P, Brugada R, Brugada J. Should patients with an asymptomatic Brugada electrocardiogram undergo pharmacological and electrophysiological testing? Circulation. 2005. 112:279–292.9. Priori SG, Napolitano C, Gasparini M, et al. Natural history of Brugada syndrome: insight for risk stratification and management. Circulation. 2002. 105:1342–1347.10. Bjerregaard P, Gussak I, Antzelevitch C. The enigmatic ECG manifestation of Brugada syndrome. J Cardiovasc Electrophysiol. 1998. 9:109–112.11. Lee MY. Brugada syndrome. Korean Circ J. 2002. 32:461–466.12. Gussak I, Antzelevitch C, Bjerregaard P, Towbin JA, Chaitman BR. The Brugada syndrome: clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol. 1999. 33:5–15.13. Guevara-Valdivia ME, de Micheli A, Iturralde P, et al. Infrequent electrocardiographic changes during exercise stress test in a patient with Brugada's syndrome. Arch Cardiol Mex. 2003. 73:212–217.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 Vaccination-Induced Ventricular Fibrillation in an Afebrile Patient With Brugada Syndrome
- Carbon monoxide poisoning-induced type 1 Brugada electrocardiographic pattern
- A Case of Idiopathic Brugada ECG Pattern Developed in Relation To Fever
- Unmasking of the Idiopathic Brugada Electrocardiogram Pattern in a Febrile Patient with Pneumonia
- In a case of female‑to‑male sex reassignment, testosterone therapy switches on an underlying Brugada