J Korean Med Sci.
2022 Oct;37(42):e306. 10.3346/jkms.2022.37.e306.
COVID-19 Vaccination-Induced Ventricular Fibrillation in an Afebrile Patient With Brugada Syndrome
- Affiliations
-
- 1Department of Cardiology, Dong-A University Hospital, Busan, Korea
- KMID: 2534759
- DOI: http://doi.org/10.3346/jkms.2022.37.e306
Abstract
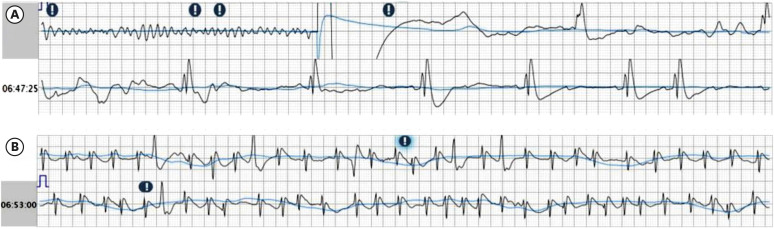
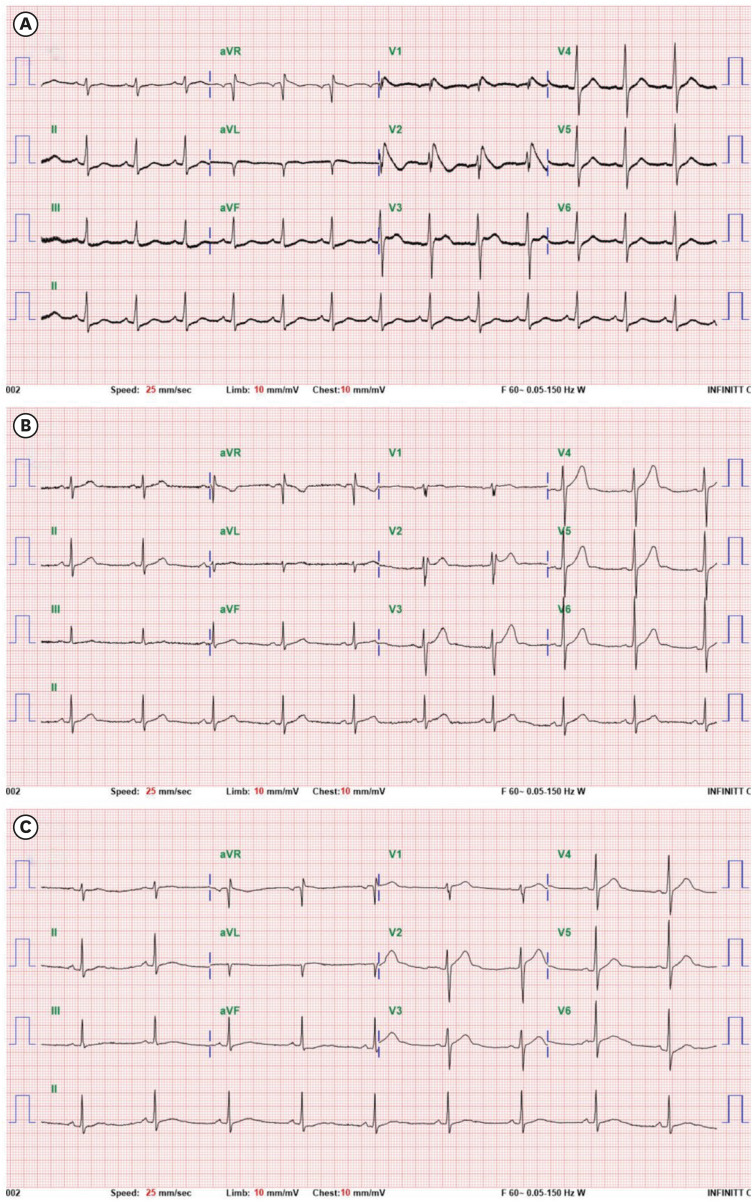
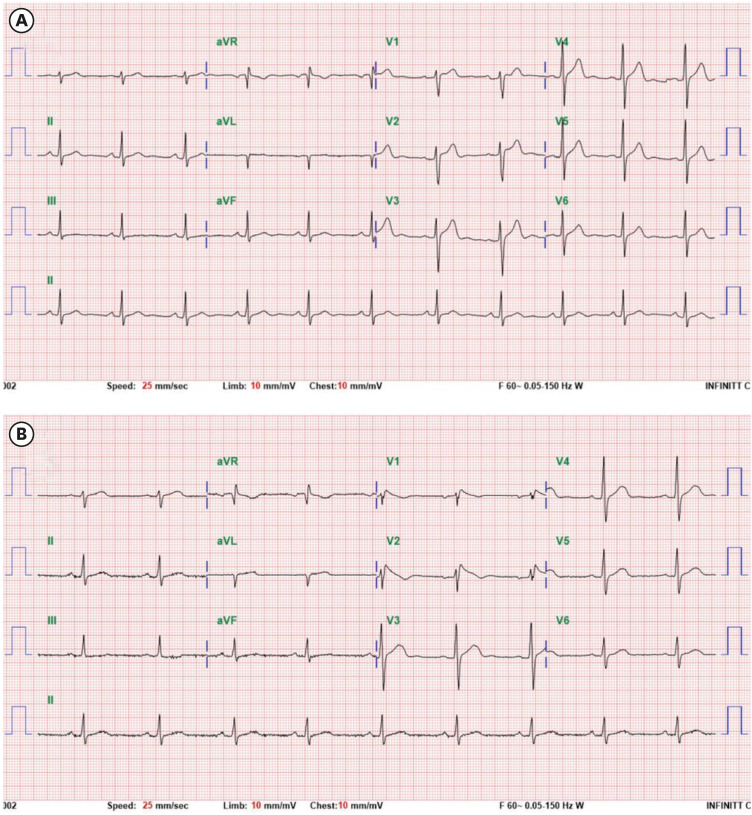
- A 43-year-old man presented with cardiac arrest 2 days after the second coronavirus disease 2019 (COVID-19) vaccination with an mRNA vaccine. Electrocardiograms showed ventricular fibrillation and type 1 Brugada pattern ST segment elevation. The patient reported having no symptoms, including febrile sensation. There were no known underlying cardiac diseases to explain such electrocardiographic abnormalities. ST segment elevation completely disappeared in two weeks. Although there were no genetic mutations or personal or family history typical of Brugada syndrome, flecainide administration induced type 1 Brugada pattern ST segment elevation. This case suggests that COVID-19 vaccination may induce cardiac ion channel dysfunction and cause life threatening ventricular arrhythmias in specific patients with Brugada syndrome.
Figure
Reference
-
1. Saha SA, Russo AM, Chung MK, Deering TF, Lakkireddy D, Gopinathannair R. COVID-19 and cardiac arrhythmias: a contemporary review. Curr Treat Options Cardiovasc Med. 2022; 24(6):87–107. PMID: 35462637.2. Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022; 28(2):410–422. PMID: 34907393.3. Chang D, Saleh M, Garcia-Bengo Y, Choi E, Epstein L, Willner J. COVID-19 Infection unmasking Brugada syndrome. HeartRhythm Case Rep. 2020; 6(5):237–240. PMID: 32292696.4. Okawa K, Kan T. Unmasked type 1 Brugada ECG pattern without a fever after a COVID-19 vaccination. HeartRhythm Case Rep. 2022; 8(4):267–269. PMID: 35079571.5. Adedeji OM, Falk Z, Tracy CM, Batarseh A. Brugada pattern in an afebrile patient with acute COVID-19. BMJ Case Rep. 2021; 14(7):e242632.6. Sorgente A, Capulzini L, Brugada P. The known into the unknown: Brugada syndrome and COVID-19. JACC Case Rep. 2020; 2(9):1250–1251. PMID: 32310242.7. Obeyesekere MN, Klein GJ, Modi S, Leong-Sit P, Gula LJ, Yee R, et al. How to perform and interpret provocative testing for the diagnosis of Brugada syndrome, long-QT syndrome, and catecholaminergic polymorphic ventricular tachycardia. Circ Arrhythm Electrophysiol. 2011; 4(6):958–964. PMID: 22203660.8. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020; 5(8):e437–e443. PMID: 32473113.9. Fazlollahi A, Zahmatyar M, Noori M, Nejadghaderi SA, Sullman MJ, Shekarriz-Foumani R, et al. Cardiac complications following mRNA COVID-19 vaccines: a systematic review of case reports and case series. Rev Med Virol. 2022; 32(4):e2318. PMID: 34921468.10. Choi S, Lee S, Seo JW, Kim MJ, Jeon YH, Park JH, et al. Myocarditis-induced sudden death after BNT162b2 mRNA COVID-19 vaccination in Korea: case report focusing on histopathological findings. J Korean Med Sci. 2021; 36(40):e286. PMID: 34664804.11. El-Battrawy I, Lang S, Zhao Z, Akin I, Yücel G, Meister S, et al. Hyperthermia influences the effects of sodium channel blocking drugs in human-induced pluripotent stem cell-derived cardiomyocytes. PLoS One. 2016; 11(11):e0166143. PMID: 27829006.12. Slater NR, Murphy KR, Sikkel MB. VT storm in long QT resulting from COVID-19 vaccine allergy treated with epinephrine. Eur Heart J. 2022; 43(11):1176. PMID: 34791122.13. Baranchuk A, Nguyen T, Ryu MH, Femenía F, Zareba W, Wilde AA, et al. Brugada phenocopy: new terminology and proposed classification. Ann Noninvasive Electrocardiol. 2012; 17(4):299–314. PMID: 23094876.14. Mulligan MJ, Lyke KE, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature. 2020; 586(7830):589–593. PMID: 32785213.15. Kim IC, Kim H, Lee HJ, Kim JY, Kim JY. Cardiac imaging of acute myocarditis following COVID-19 mRNA vaccination. J Korean Med Sci. 2021; 36(32):e229. PMID: 34402228.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Brugada Syndrome
- Anesthetic Management of a Patient with Brugada Syndrome: A case report
- Anesthetic Experience for Trans-Sphenoidal Surgery of Pituitary Adenoma on a Patient with Brugada Syndrome: A Case Report
- A Concealed Brugada Electrocardiogram Pattern Revealed after Administering Propafenone to a Patient with Atrial Fibrillation
- Spinal Anesthesia of a Patient with Brugada Syndrome: A case report