Korean Circ J.
2008 Mar;38(3):140-143. 10.4070/kcj.2008.38.3.140.
Noninvasive Pacemaker Stress Echocardiography as a Screening Test for Coronary Artery Disease in Patients With Atypical Angina and Permanent Pacemaker
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. heartswjin@yahoo.co.kr
- KMID: 2225830
- DOI: http://doi.org/10.4070/kcj.2008.38.3.140
Abstract
- BACKGROUND AND OBJECTIVES
Making the noninvasive diagnosis of coronary artery disease in patients with a permanent pacemaker is difficult because of the inability to interpret electrocardiograms and the low specificity of perfusion scintigraphy. We evaluated the diagnostic accuracy of noninvasive pacemaker stress echocardiography (PASE) as a screening test for coronary artery disease in patients with atypical angina and a permanent pacemaker.
SUBJECTS AND METHODS
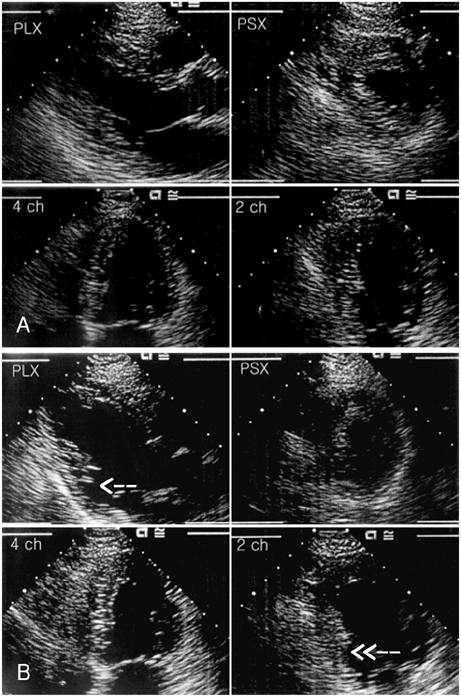
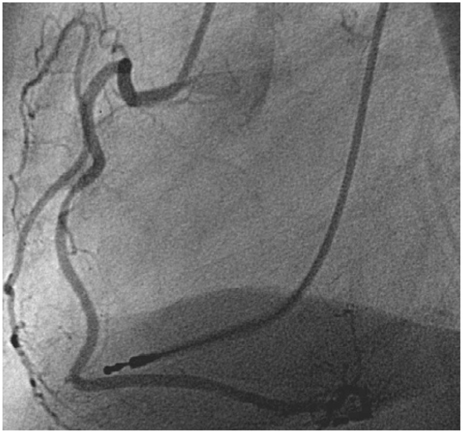
This a prospective study, and transthoracic stress-pacing echocardiography was performed on 15 patients (9 men and 6 women; age, mean age: 71.1+/-11.0 years) with atypical angina and a permanent pacemaker. All the patients underwent noninvasive pacemaker-stress echocardiography by external programming (pacing the heart rate up to 150 beats per minute). Coronary angiography was performed on the 8 patients with positive PASE results. Significant coronary artery disease was defined as > or =70% stenosis in at least one major coronary artery.
RESULTS
The echocardiographic images were interpretable for all the patients. No significant side effects were observed. The left ventricular systolic function was preserved in all the patients (left ventricular ejection fraction; 63.5+/-8%). Only 5 (62.5%) of 8 patients showed significant coronary artery disease, as documented by coronary angiography.
CONCLUSION
Noninvasive PASE is a simple, rapid, safe and diagnostically efficient test for detecting coronary artery disease in patients with atypical angina and a permanent pacemaker. Larger studies are necessary to validate our findings.
MeSH Terms
Figure
Reference
-
1. Chaitman BR. Braunwald E, editor. Exercise stress testing. Heart Disease: A Textbook of Cardiovascular Medicine. 2001. 6th ed. Philadelphia: Saunders;129–155.2. Lakkis NM, He ZX, Verani MS. Diagnosis of coronary artery disease by exercise thallium-201 tomography in patients with a right ventricular pacemaker. J Am Coll Cardiol. 1997. 29:1221–1225.3. Skalidis EI, Kochiadakis GE, Koukouraki SI, et al. Myocardial perfusion in patients with permanent ventricular pacing and normal coronary arteries. J Am Coll Cardiol. 2001. 37:124–129.4. Benchimol D, Mozanof M, Dubroca B, et al. Detection of coronary stenoses by stress echocardiography using a previously implanted pacemaker for ventricular pacing: preliminary report of a new method. Clin Cardiol. 2000. 23:842–848.5. Picano E, Alaimo A, Chubuchny V, et al. Noninvasive pacemaker stress echocardiography for diagnosis of coronary artery disease: a multicenter study. J Am Coll Cardiol. 2002. 40:1305–1310.6. Armstrong WF, Pellikka PA, Ryan T, Crouse L, Zoghbi WA. Stress echocardiography: recommendations for performance and interpretation of stress echocardiography. J Am Soc Echocardiogr. 1998. 11:97–104.7. Choi SJ, Kim HS, Seo JD. Identification of ischemic myocardium with simultaneous dobutamine stress echocardiography and 99mTC-MIBI SPECT in patients with suspected coronary artery disease. Korean Circ J. 1993. 23:960–971.8. Tzivoni D, Weiss AT, Solomon J, et al. Diagnosis of coronary artery disease by multigated radionuclide angiography during right atrial pacing. Chest. 1981. 80:562–565.9. Chapman PD, Doyle TP, Troup PJ, Gross CM, Wann LS. Stress echocardiography with transesophageal atrial pacing: preliminary report of a new method for detection of ischemic wall motion abnormalities. Circulation. 1984. 70:445–450.10. Atar S, Nagai T, Cercek B, Nagvi TZ, Luo H, Siegel RJ. Pacing stress echocardiography: an alternative to pharmacologic stress testing. J Am Coll Cardiol. 2000. 36:1935–1941.11. Marangelli V, Iliceto S, Piccinni G, De Martino G, Sorgente L, Rizzon P. Detection of coronary artery disease by digital stress echocardiography: comparison of exercise, transesophageal atrial pacing and dipyridamole echocardiography. J Am Coll Cardiol. 1994. 24:117–124.12. Schroder K, Voller H, Dingerkus H, et al. Comparison of the diagnostic potential of four echocardiographic stress tests shortly after acute myocardial infarction: submaximal exercise, transesophageal atrial pacing, dipyridamole, and dobutamine-atropine. Am J Cardiol. 1996. 77:909–914.13. Gong G, Ugurbil K, Zhang J. Transmural metabolic heterogeneity at high cardiac work states. Am J Physiol. 1999. 277:H236–H242.14. Takeuchi M, Nohtomi Y, Kuroiwa A. Effect of ventricular pacing on coronary blood flow in patients with normal coronary arteries. Pacing Clin Electrophysiol. 1997. 20:2463–2469.15. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block: the effect of interventricular asynchrony. Circulation. 1989. 79:845–853.16. Picano E. Stress Echocardiography. 2003. 4th ed. Heidelberg: Springer Verlag.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reversibility of Atrioventricular Block According to Coronary Artery Disease: Results of a Retrospective Study
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality
- Extraction of an Infected Permanent Pacemaker Lead UsingCardiopulmonary Bypass: 2 case reports
- The Usefulness of Exercise Stress Echocardiography in Diagnosis of Coronary Artery Disease
- Permanent Pacemaker Lead Induced Severe Tricuspid Regurgitation in Patient Undergoing Multiple Valve Surgery