Korean Circ J.
2008 Apr;38(4):191-196. 10.4070/kcj.2008.38.4.191.
The Clinical Effects and Radial Artery Vasodilation After High Dose Nicorandil Solution During Coronary Angiography via the Radial Artery
- Affiliations
-
- 1Cardiovascular Center, Gwangju Veterans Hospital, Gwangju, Korea. mlovekw@hanmail.net
- KMID: 2225816
- DOI: http://doi.org/10.4070/kcj.2008.38.4.191
Abstract
-
BACKGROUND AND OBJECTIVES: A spasm of the radial artery is one of the most common complications of coronary angiography (CAG) via the transradial approach (TR), and this spasm sometimes disturbs the procedure. Nicorandil has recently shown dose-dependent dilatation of the blood vessels and ischemic preconditioning. This study was designed to evaluate the clinical effects and radial artery vasodilation of high dose nicorandil solution during CAG via the radial artery.
SUBJECTS AND METHODS
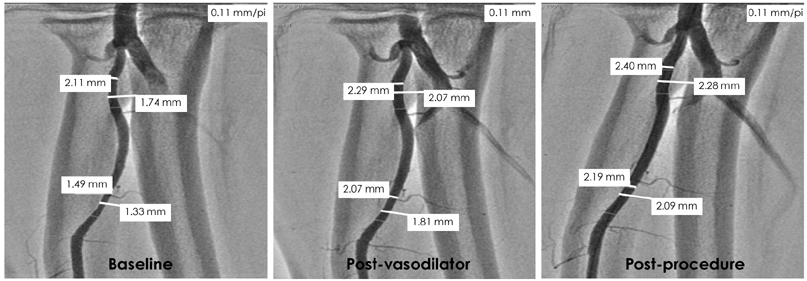
This study was a prospective, randomized study to compare the effects of 12 mg of nicorandil (the Nicorandil group) and 10 mL of a cocktail solution (nitroglycerine 200 microgram mixed with verapamil 100 microgram) (the Cocktail group) in 146 patients. Vasospasms, which were expressed as the stenosis of the radial artery were examined at 2 parts of the radial artery.
RESULTS
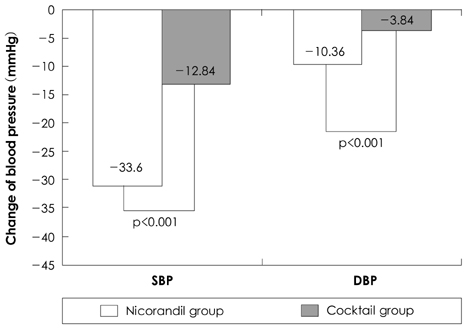
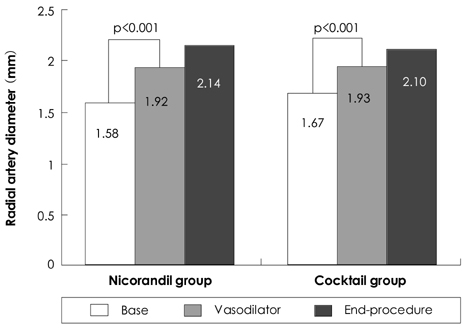
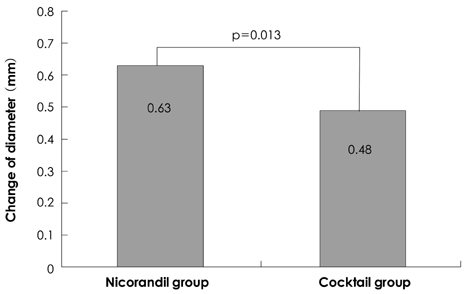
There were no significant difference of gender, age and risk factors for the 2 groups of patients. The reductions in the systolic and diastolic blood pressure (BP) 1 minute after drug administration were 33.6+/-11.4/10.4+/-7.7 mmHg in the Nicorandil group and 12.8+/-9.8/3.8+/-5.3 mmHg in the Cocktail group (p<0.001). Both vasodilating agents showed significant radial artery vasodilation after administration of the drugs (p<0.005 for all). The minimal luminal diameter (MLD) after drug administration was more dilated in the Nicorandil group than that in the Cocktail group (0.63+/-0.25 mm vs. 0.48+/-0.19 mm, respectively, p=0.013).
CONCLUSION
Nicorandil solution was more effective for inducing vasodilation of the radial artery, but it was not clinical superior to the cocktail solution.
Keyword
MeSH Terms
Figure
Reference
-
1. Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn. 1989. 16:3–7.2. Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet Cardiovasc Diagn. 1993. 30:173–178.3. Valsecchi O, Musumeci G, Vassileva A, et al. Safety and feasibility of transradial coronary angioplasty in elderly patients. Ital Heart J. 2004. 5:926–931.4. Han KR, Park WJ, Oh DJ, et al. Feasibility and problems in transradial coronary angiography and intervention. Korean Circ J. 2000. 30:1083–1091.5. Sakata Y, Kodama K, Komamura K, et al. Salutary effect of adjunctive intracoronary nicorandil administration on restoration of myocardial blood flow and functional improvement in patients with acute myocardial infarction. Am Heart J. 1997. 133:616–621.6. Taira N. Nicorandil as a hybrid between nitrates and potassium channel activators. Am J Cardiol. 1989. 63:18J–24J.7. Auchampach JA, Cavero I, Gross GJ. Nicorandil attenuates myocardial dysfunction associated with transient ischemia by opening ATP-dependent potassium channels. J Cardiovasc Pharmacol. 1992. 20:765–771.8. Kempsford RD, Hawgood BJ. Assessment of the antiarrhythmic activity of nicorandil during myocardial ischemia and reperfusion. Eur J Pharmacol. 1989. 163:61–68.9. Ishii H, Ichimiya S, Kanashiro M, et al. Impact of a single intravenous administration of nicorandil before reperfusion in patients with ST-segment-elevation myocardial infarction. Circulation. 2005. 112:1284–1288.10. Murayama S, Yamakado T, Nakano T. Effects of nicorandil, an antianginal potassium channel opener, on left ventricular systolic and diastolic function in patients with chronic coronary artery disease. Am J Cardiol. 1997. 79:1685–1689.11. Kato K. Haemodynamic and clinical effects of an intravenous potassium channel opener: a review. Eur Heart J. 1993. 14:Suppl B. 40–47.12. Kim SH, Kim EJ, Kim MK, et al. Comparison of the effects of nicorandil and cocktail solution to prevent radial artery spasm during coronary angiography. Korean Circ J. 2006. 36:133–139.13. Fukuda N, Iwahara S, Harada A, et al. Vasospasms of the radial artery after the transradial approach for coronary angiography and angioplasty. Jpn Heart J. 2004. 45:723–731.14. Hildick-Smith DJ, Lowe MD, Walsh JT, et al. Coronary angiography from the radial artery: experience, complications and limitation. Int J Cardiol. 1998. 64:231–239.15. Cable DG, Caccitolo JA, Pfeifer WA, et al. Endothelial regulation of vascular contraction in radial and internal mammary arteries. Ann Thorac Surg. 1999. 67:1083–1090.16. Chardigny C, Jebara VA, Acar C, et al. Vasoreactivity of the radial artery: comparison with the internal mammary and gastroepiploic arteries with implication for coronary artery surgery. Circulation. 1993. 88:II115–II127.17. Chamiot-Clerc P, Copie X, Renaud JF, Safar M, Girerd X. Comparative reactivity and mechanical properties of human isolated internal mammary and radial arteries. Cardiovasc Res. 1998. 37:811–819.18. Koga S, Ikeda S, Futagawa K, et al. The use of a hydrophilic-coated catheter during transradial cardiac catheterization is associated with a low incidence of radial artery spasm. Int J Cardiol. 2004. 96:255–258.19. Shapira OM, Xu A, Vita JA, et al. Nitroglycerin is superior to diltiazem as a coronary bypass conduit vasodilator. J Thorac Cardiovasc Surg. 1999. 117:906–911.20. Mont'Alverne Filho JR, Assad JA, Zago Ado C, et al. Comparative study of the use of diltiazem as an antispasmodic drug in coronary angiography via the transradial approach. Arq Bras Cardiol. 2003. 81:59–63.21. Kiemeneij F, Vajifdar BU, Eccleshall SC, et al. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Cathet Cardiovasc Intervent. 2003. 58:281–284.22. He GW, Yang CQ. Use of verapamil and nitroglycerin solution in preparation of radial artery for coronary grafting. Ann Thorac Surg. 1996. 61:610–614.23. Ueda K, Goto C, Jitsuiki D, et al. The nicorandil-induced vasodilation in humans is inhibited by miconazole. J Cardiovasc Pharmacol. 2005. 45:290–294.24. Sadaba JR, Mathew K, Munsch CM, Beech DJ. Vasorelaxant properties of nicorandil on human radial artery. Eur J Cardiothorac Surg. 2000. 17:319–324.25. IONA Study Group. Effect of nicorandil on coronary events in patients with stable angina. Lancet. 2002. 359:1269–1275.26. Kim JH, Jeong MH, Lim SY, et al. The clinical effects of nicorandil during percutaneous coronary intervention in patients with unstable angina. Korean Circ J. 2005. 35:322–327.27. Kim SM, Kim DK, Kim DI, Kim DS, Joo SJ, Lee JW. Novel diagnostic catheter specifically designed for both coronary arteries via the right transradial approach. INT J Cardiovasc Imaging. 2006. 22:295–303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Effects of Nicorandil and Cocktail Solution to Prevent Radial Artery Spasm during Coronary Angiography
- Feasibility and Problems in Transradial Coronary Angiography and Intervention
- The Study of Branching Anomaly and Tortuosity of Radial Artery for Trans-Radial Coronary Procedure
- Iatrogenic radial artery perforation during transradial coronary angiography
- Harvesting of Radial Artery With Harmonic Scalpel