The Significance of Clopidogrel Low-Responsiveness on Stent Thrombosis and Cardiac Death Assessed by the Verifynow P2Y12 Assay in Patients With Acute Coronary Syndrome Within 6 Months After Drug-Eluting Stent Implantation
- Affiliations
-
- 1Division of Cardiology, Gachon University of Medicine and Science, Gil Medical Center, Incheon, Korea.
- 2Division of Cardiology, Yonsei University Wonju College of Medicine, Wonju, Korea. carshlee@yonsei.ac.kr
- KMID: 2225638
- DOI: http://doi.org/10.4070/kcj.2009.39.12.512
Abstract
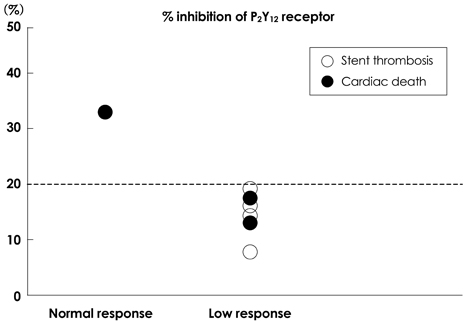
- BACKGROUND AND OBJECTIVES
Clopidogrel resistance or low-responsiveness may be associated with recurrent atherothrombotic events after drug-eluting stent (DES) implantation. We prospectively evaluated the association between clopidogrel resistance assessed by the Verifynow(TM) P2Y12 assay (Accumetrics, San Diego, CA, USA) and stent thrombosis (ST) or cardiac death (CD) in patients with acute coronary syndrome (ACS) within 6 months after DES implantation. SUBJECTS AND METHODS: We enrolled 237 consecutive patients (160 males, 65.2+/-10.3 years) with ACS who received a DES implantation. The composite endpoint was defined to CD or ST by Academic Research Consortium definitions within 6 months post-implantation. Clopidogrel resistance was defined as <20% inhibition of the P2Y12 receptor. RESULTS: Baseline demographic characteristics were similar between 142 normal individuals and 95 clopidogrel resistant patients. CD occurred in one case (0.7%) in the normal group and two cases (2.13%) in the resistant group (p=0.344). There was no episode of ST in the normal group and four episodes in the resistant group (4.2%, four definite ST) (p=0.035). Univariate logistic regression revealed an adjusted odds ratio (OR) for composite end point of CD or ST of 9.646 {95% confidence interval (CI) 1.139-81.679}, and multivariate logistic regression for composite end point revealed an OR of 12.074 (95% CI 1.205-120.992). CONCLUSION: Clopidogrel low-responsiveness assessed by the Verifynow(TM) P2Y12 assay is an independent predictor of ST and composite end point of ST or CD in patients with ACS within 6 months after DES implantation.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Correlations between High Platelet Reactivity, Extent of Coronary Artery Disease, and Periprocedural Myonecrosis in Patients with Acute Coronary Syndrome
Kyeong Ho Yun, Jum Suk Ko, Jeong Mi Lee, Sang Jae Rhee
Chonnam Med J. 2017;53(2):147-152. doi: 10.4068/cmj.2017.53.2.147.Effects of 600 mg versus 300 mg Loading Dose of Clopidogrel in Asian Patients with ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention: Long-Term Follow-Up Study
Pil Sang Song, Joo-Yong Hahn, Young Bin Song, Jin-Ho Choi, Seung-Hyuk Choi, Gu Hyun Kang, Kye Taek Ahn, Woo-Hyun Lim, Kyung Woo Park, Hyo-Soo Kim, Hyeon-Cheol Gwon
Yonsei Med J. 2012;53(5):906-914. doi: 10.3349/ymj.2012.53.5.906.Adjunctive Cilostazol versus High Maintenance Dose of Clopidogrel in Patients with Hyporesponsiveness to Chronic Clopidogrel Therapy
Ga Yeon Lee, Joo-Yong Hahn, Soo-Youn Lee, Hee-Jin Kim, Jun Hyung Kim, Sang-Yup Lee, Young Bin Song, Seung-Hyuk Choi, Jin-Ho Choi, Hyeon-Cheol Gwon
Yonsei Med J. 2013;54(1):34-40. doi: 10.3349/ymj.2013.54.1.34.Determination of the Prevalence of Aspirin and Clopidogrel Resistances in Patients with Coronary Artery Disease by using Various Platelet-function Tests
Kwang-Sook Woo, Bo-Ram Kim, Ji-Eun Kim, Ri-Young Goh, Long-Hao Yu, Moo-Hyun Kim, Jin-Yeong Han
Korean J Lab Med. 2010;30(5):460-468. doi: 10.3343/kjlm.2010.30.5.460.
Reference
-
1. Serruys PW, de Jaegere P, Kiemeneij F, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994. 331:489–495.2. Fischman DL, Leon MB, Baim DS, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994. 331:496–501.3. Babapulle MN, Joseph L, Belisle P, Brophy JM, Eisenberg MJ. A hierarchical Bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet. 2004. 364:583–591.4. Schampaert E, Cohen EA, Schluter M, et al. The Canadian study of the sirolimus-eluting stent in the treatment of patients with long de novo lesions in small native coronary arteries (C-SIRIUS). J Am Coll Cardiol. 2004. 43:1110–1115.5. Schofer J, Schluter M, Gershlick AH, et al. Sirolimus-eluting stents for treatment of patients with long atherosclerotic lesions in small coronary arteries: double-blind, randomised controlled trial (E-SIRIUS). Lancet. 2003. 362:1093–1099.6. Park SJ, Kim YH, Lee BK, et al. Sirolimus-eluting stent implantation for unprotected left main coronary artery stenosis: comparison with bare metal stent implantation. J Am Coll Cardiol. 2005. 45:351–356.7. Jeremias A, Sylvia B, Bridges J, et al. Stent thrombosis after successful sirolimus-eluting stent implantation. Circulation. 2004. 109:1930–1932.8. De Luca G, Carbone G, Maione A, Gregorio G. In-stent thrombosis after discontinuation of antiplatelet therapy 2 years after DES implantation: a case report. Int J Cardiol. 2007. 116:399–400.9. Artang R, Dieter RS. Analysis of 36 reported cases of late thrombosis in drug-eluting stents placed in coronary arteries. Am J Cardiol. 2007. 99:1039–1043.10. Grines CL, Bonow RO, Casey DE Jr, et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. Catheter Cardiovasc Interv. 2007. 69:334–340.11. Eikelboom JW, Hirsh J, Weith JI, et al. Aspirin-resistant thromboxane biosynthesis and the risk of myocardiac infarction, stroke or cordiovascular death in patients at high risk for cardiovascular events. Circulation. 2002. 105:1650–1655.12. Gum PA, Kottke-Morchant K, Poggio ED, et al. Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol. 2001. 88:230–235.13. Gusbel PA, Bilden KP, Hiatt BL, et al. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation. 2003. 107:2908–2913.14. Serebruary VL, Steingubl SR, Berger PB, et al. Variability in platelet responsivent to clopidogrel among 544 individuals. J Am Coll Cordiol. 2005. 45:246–251.15. Cutlip DE, Baim DS, Ho KK, et al. Stent thrombosis in the modern era: a pooled analysis of multicenter coronary stent clinical trials. Circulation. 2001. 103:1967–1971.16. Wiviott SD, Antman EM. Clopidogrel resistance: a new chapter in a fast-moving story. Circulation. 2004. 109:3064–3067.17. Matetzky S, Shenkman B, Guetta V, et al. Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation. 2004. 109:3171–3175.18. van Werkum JW, van der Stelt CA, Seesing TH, Hackeng CM, ten Berg JM. A head-to-head comparison between the VerifyNow P2Y12 assay and light transmittance aggregometry for monitoring the individual platelet response to clopidogrel in patients undergoing elective percutaneous coronary intervention. J Thromb Haemost. 2006. 4:2516–2518.19. Malinin A, Pokov A, Swaim L, Kotob M, Serebruany V. Validation of a VerifyNow-P2Y12 cartridge for monitoring platelet inhibition with clopidogrel. Methods Find Exp Clin Pharmacol. 2006. 28:315–322.20. Paniccia R, Antonucci E, Gori AM, et al. Different methodologies for evaluating the effect of clopidogrel on platelet function in high-risk coronary artery disease patients. J Thromb Haemost. 2007. 5:1839–1847.21. Lev EI, Patel RT, Maresh KJ, et al. Aspirin and clopidogrel drug response in patients undergoing percutaneous coronary intervention: the role of dual drug resistance. J Am Coll Cardiol. 2006. 47:27–33.22. Gurbel PA, Bliden KP, Zaman KA, Yoho JA, Hayes KM, Tantry US. Clopidogrel loading with eptifibatide to arrest the reactivity of platelets: results of the Clopidogrel Loading With Eptifibatide to Arrest the Reactivity of Platelets (CLEAR PLATELETS) study. Circulation. 2005. 111:1153–1159.23. Cuisset T, Frere C, Quilici J, et al. High post-treatment platelet reactivity identified low-responders to dual antiplatelet therapy at increased risk of recurrent cardiovascular events after stenting for acute coronary syndrome. J Thromb Haemost. 2006. 4:542–549.24. Geisler T, Langer H, Wydymus M, et al. Low response to clopidogrel is associated with cardiovascular outcome after coronary stent implantation. Eur Heart J. 2006. 27:2420–2425.25. Gurbel PA, Bliden KP, Guyer K, et al. Platelet reactivity in patients and recurrent events post-stenting: results of the PREPARE POST-STENTING Study. J Am Coll Cardiol. 2005. 46:1820–1826.26. Samara WM, Bliden KP, Tantry US, Gurbel PA. The difference between clopidogrel responsiveness and posttreatment platelet reactivity. Thromb Res. 2005. 115:89–94.27. Buonamici P, Marcucci R, Migliorini A, et al. Impact of platelet reactivity after clopidogrel administration on drug-eluting stent thrombosis. J Am Coll Cardiol. 2007. 49:2312–2317.28. Farb A, Boam AB. Stent thrombosis redux: the FDA perspective. N Engl J Med. 2007. 356:984–987.29. Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drugeluting stents. JAMA. 2005. 293:2126–2130.30. Park DW, Park SW. Stent thrombosis in the era of the drug-eluting stent. Korean Circ J. 2005. 35:791–794.31. Park S, Hong GR, Seo HS, Tahk SJ. Stent thrombosis after successful drug-eluting stent implantation. Korean Circ J. 2005. 35:163–171.32. Nam CW, Kim KB, Hur SH, et al. Impact of optimal stent expansion on late outcomes after sirolimus-eluting stent implantation: an intravascular ultrasound study. Korean Circ J. 2007. 37:244–250.33. Fujii K, Carlier SG, Mintz GS, et al. Stent underexpansion and residual reference segment stenosis are related to stent thrombosis after sirolimus-eluting stent implantation: an intravascular ultrasound study. J Am Coll Cardiol. 2005. 45:995–998.34. Foussas SG, Zairis MN, Patsourakos NG, et al. The impact of oral antiplatelet responsiveness on the long-term prognosis after coronary stenting. Am Heart J. 2007. 154:676–681.35. Price MJ, Endemann S, Gollapudi RR, et al. Prognostic significance of post-clopidogrel platelet reactivity assessed by a pointof-care assay on thrombotic events after drug-eluting stent implantation. Eur Heart J. 2008. 29:992–1000.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Very Late Stent Thrombosis in Coronary Bare-Metal Stent Implantation: A Case Report
- A Case of Stent Thrombosis Occurred at 5 Years after Sirolimus-Eluting Stent Implantation
- Simultaneous Multivessel Acute Stent Thrombosis in a Patient with Gastrointestinal Bleeding
- A Case of Ticagrelor Rescue Therapy in a Patient with Subacute Stent Thrombosis
- Very Late Stent Thrombosis after Drug-Eluting Stent Implantation in a Patient without Aspirin and Clopidogrel Resistance