Korean Circ J.
2013 Aug;43(8):519-526. 10.4070/kcj.2013.43.8.519.
One-Year Clinical Outcomes among Patients with Metabolic Syndrome and Acute Myocardial Infarction
- Affiliations
-
- 1Chonnam National University Hospital, Gwangju, Korea. myungho@chollian.net
- 2Yeungnam University Hospital, Daegu, Korea.
- 3Kyungpook National University Hospital, Daegu, Korea.
- 4Pusan National University Hospital, Busan, Korea.
- 5Chungnam National University Hospital, Daejeon, Korea.
- 6Chunbuk National University Hospital, Jeonju, Korea.
- 7Kyung Hee University Hospital, Seoul, Korea.
- 8Chungbuk National University Hospital, Cheongju, Korea.
- 9Korea University Guro Hospital, Seoul, Korea.
- 10Konyang University, Daejeon, Korea.
- 11The Catholic University of Korea, Seoul St. Mary's Hospital, Seoul, Korea.
- 12Asan Medical Center, Seoul, Korea.
- 13Korea Cardiovascular Stent Research Institute of Chonnam National University, Gwangju, Korea.
- KMID: 2224841
- DOI: http://doi.org/10.4070/kcj.2013.43.8.519
Abstract
- BACKGROUND AND OBJECTIVES
Metabolic syndrome (MetS) is an important risk factor for cardiovascular disease. However, the clinical outcome of acute myocardial infarction (AMI) with MetS has not been well examined. The purpose of this study was to evaluate the clinical outcomes of AMI patients with MetS.
SUBJECTS AND METHODS
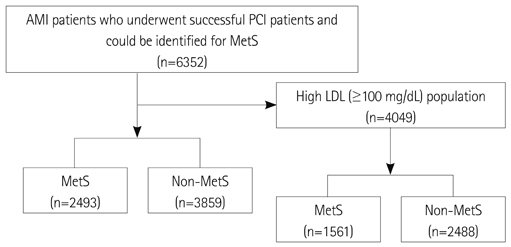
We evaluated a total of 6352 AMI patients who had successful percutaneous coronary interventions and could be identified for MetS between 2005 and 2008 at 51 hospitals participating in the Korea Acute Myocardial Infarction Registry. They were divided into 2 groups according to the presence of MetS: the MetS group (n=2493, 39.2%) versus the Non-MetS group (n=3859, 60.8%). In addition, 4049 AMI patients with high levels of low density lipoprotein-cholesterol (LDL-C) (> or =100 mg/dL) among them, were divided into the MetS group (n=1561, 38.6%) versus the Non-MetS group (n=2488, 61.4%).
RESULTS
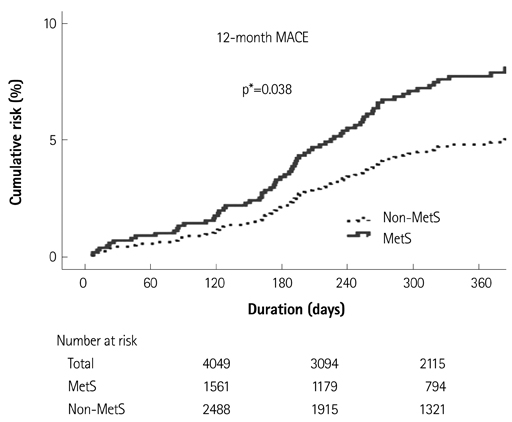
In the overall population, there was no significant difference in 12-month the major adverse cardiac events (MACE) rate between the 2 groups. However, the MetS group showed a significantly higher 12-month MACE rate in the high LDL-C population. Multivariate analysis showed that MetS was an independent prognostic factor for 12-month MACE {hazard ratio (HR) 1.607, 95% confidence interval (CI) 1.027 to 2.513, adjusted p=0.038} and for 12-month target vessel revascularization (HR 1.564, 95% CI 1.092 to 2.240, adjusted p=0.015) in the high LDL-C population.
CONCLUSION
MetS patients with AMI in the overall population showed no significant difference in 12-month clinical outcomes. However, in patients with higher LDL-C > or =100 mg/dL, they showed significantly worse clinical outcome than Non-MetS patients. Therefore, it is important to ascertain the presence of MetS in AMI patients, and more aggressive therapy should be strongly considered for AMI patient with MetS.
MeSH Terms
Figure
Reference
-
1. Skilton MR, Moulin P, Sérusclat A, Nony P, Bonnet F. A comparison of the NCEP-ATPIII, IDF and AHA/NHLBI metabolic syndrome definitions with relation to early carotid atherosclerosis in subjects with hypercholesterolemia or at risk of CVD: evidence for sex-specific differences. Atherosclerosis. 2007; 190:416–422.2. Lorenzo C, Okoloise M, Williams K, Stern MP, Haffner SM. San Antonio Heart Study. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study. Diabetes Care. 2003; 26:3153–3159.3. Girman CJ, Rhodes T, Mercuri M, et al. The metabolic syndrome and risk of major coronary events in the Scandinavian Simvastatin Survival Study (4S) and the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS). Am J Cardiol. 2004; 93:136–141.4. Selcuk H, Temizhan A, Selcuk MT, et al. Impact of metabolic syndrome on future cardiovascular events in patients with first acute myocardial infarction. Coron Artery Dis. 2009; 20:370–375.5. Karthikeyan G, Teo KK, Islam S, et al. Lipid profile, plasma apolipoproteins, and risk of a first myocardial infarction among Asians: an analysis from the INTERHEART Study. J Am Coll Cardiol. 2009; 53:244–253.6. Sim DS, Jeong MH, Kang JC. Current management of acute myocardial infarction: experience from the Korea Acute Myocardial Infarction Registry. J Cardiol. 2010; 56:1–7.7. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752.8. Zeller M, Steg PG, Ravisy J, et al. Prevalence and impact of metabolic syndrome on hospital outcomes in acute myocardial infarction. Arch Intern Med. 2005; 165:1192–1198.9. Lee MG, Jeong MH, Ahn Y, et al. Impact of the metabolic syndrome on the clinical outcome of patients with acute ST-elevation myocardial infarction. J Korean Med Sci. 2010; 25:1456–1461.10. Kim JS, Lee HC, Choi BK, et al. Impact of metabolic syndrome on instent restenosis and clinical outcomes after percutaneous coronary stent implantation. Diabetes Res Clin Pract. 2010; 88:e38–e41.11. Hoffmann R, Stellbrink E, Schröder J, et al. Impact of the metabolic syndrome on angiographic and clinical events after coronary intervention using bare-metal or sirolimus-eluting stents. Am J Cardiol. 2007; 100:1347–1352.12. Rana JS, Monraats PS, Zwinderman AH, et al. Metabolic syndrome and risk of restenosis in patients undergoing percutaneous coronary intervention. Diabetes Care. 2005; 28:873–877.13. Xu D, Guo Y, Wang H, et al. The angiographic and clinical outcomes after coronary stenting in patients with metabolic syndrome. Atherosclerosis. 2012; 221:416–421.14. Ascaso J, Gonzalez Santos P, Hernandez Mijares A, et al. Management of dyslipidemia in the metabolic syndrome: recommendations of the Spanish HDL-Forum. Am J Cardiovasc Drugs. 2007; 7:39–58.15. Fukushima Y, Hirayama S, Ueno T, et al. Small dense LDL cholesterol is a robust therapeutic marker of statin treatment in patients with acute coronary syndrome and metabolic syndrome. Clin Chim Acta. 2011; 412:1423–1427.16. Koba S, Yokota Y, Hirano T, et al. Small LDL-cholesterol is superior to LDL-cholesterol for determining severe coronary atherosclerosis. J Atheroscler Thromb. 2008; 15:250–260.17. Moon JY, Kwon HM, Kwon SW, et al. Lipoprotein(a) and LDL particle size are related to the severity of coronary artery disease. Cardiology. 2007; 108:282–289.18. Yazdandoust S, Parizadeh SM, Moohebati M, et al. Serum small dense low-density lipoprotein concentrations are elevated in patients with significant coronary artery stenosis and are related to features of the metabolic syndrome. Lipids. 2012; 47:963–972.19. Goswami B, Rajappa M, Singh B, Ray PC, Kumar S, Mallika V. Inflammation and dyslipidaemia: a possible interplay between established risk factors in North Indian males with coronary artery disease. Cardiovasc J Afr. 2010; 21:103–108.20. Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr. 2006; 83:461S–465S.21. Goyal SN, Bharti S, Krishnamurthy B, Agrawal Y, Ojha SK, Arya DS. Impact of metabolic syndrome on re-stenosis development: role of drug-eluting stents. Diab Vasc Dis Res. 2012; 9:177–188.22. Deedwania PC, Hunninghake DB, Bays HE, et al. Effects of rosuvastatin, atorvastatin, simvastatin, and pravastatin on atherogenic dyslipidemia in patients with characteristics of the metabolic syndrome. Am J Cardiol. 2005; 95:360–366.23. Baldassarre S, Scruel O, Deckelbaum RJ, Dupont IE, Ducobu J, Carpentier YA. Beneficial effects of atorvastatin on sd LDL and LDL phenotype B in statin-naive patients and patients previously treated with simvastatin or pravastatin. Int J Cardiol. 2005; 104:338–345.24. Bahadir MA, Oguz A, Uzunlulu M, Bahadir O. Effects of different statin treatments on small dense low-density lipoprotein in patients with metabolic syndrome. J Atheroscler Thromb. 2009; 16:684–690.25. Devaraj S, Chan E, Jialal I. Direct demonstration of an antiinflammatory effect of simvastatin in subjects with the metabolic syndrome. J Clin Endocrinol Metab. 2006; 91:4489–4496.26. Ray KK, Cannon CP. Intensive statin therapy in acute coronary syndromes: clinical benefits and vascular biology. Curr Opin Lipidol. 2004; 15:637–643.27. Filardi PP, Cecere M, Savarese G, et al. [Inflammation and lipids in the coronary pathology. Risk factors, causes or therapeutic target?]. G Ital Cardiol (Rome). 2010; 11:12 Suppl 3. 10S–15S.28. Ulus T, Parspour A, Cavusoglu Y, Entok E, Uslu I, Demirustu C. Statins improve myocardial perfusion in metabolic syndrome patients who have perfusion defects on myocardial perfusion imaging and angiographically normal coronary arteries. Eur Rev Med Pharmacol Sci. 2012; 16:328–334.29. Murrow JR, Sher S, Ali S, et al. The differential effect of statins on oxidative stress and endothelial function: atorvastatin versus pravastatin. J Clin Lipidol. 2012; 6:42–49.30. Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). Steg PG, James SK, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012; 33:2569–2619.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Invasive Treatment of Acute Myocardial Infarction: What is the Optimal Therapy for Acute Myocardial Infarction?
- The Eletrocardiographic Analysis of Acute Myocardial Infarction and Non-infarction Syndrome In the Patients with ST Segment Elevation and Chest Pain
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea
- A Case of Pericardial Effusion after Acute Myocardial Infarction
- Spontaneous Pulmonary Hemorrhage and Adult Respiratory Distress Syndrome after Thrombolytic Therapy for Acute Myocardial Infarction