Korean Circ J.
2013 Nov;43(11):725-730. 10.4070/kcj.2013.43.11.725.
Influence of the Timing of Percutaneous Coronary Intervention on Clinical Outcomes in Non-ST-Elevation Myocardial Infarction
- Affiliations
-
- 1Department of Cardiology, Batman State Hospital, Batman, Turkey. kamurantekin@gmail.com
- 2Department of Cardiology, Adanana Numune Education and Research Hospital, Istanbul, Turkey.
- KMID: 2224803
- DOI: http://doi.org/10.4070/kcj.2013.43.11.725
Abstract
- BACKGROUND AND OBJECTIVES
We have intended to investigate the influence of the timing of invasive procedures on all-cause mortality, recurrent myocardial infarction (MI), re-hospitalization due to cardiac causes and left ventricular function over a 3-month period among patients with Non-ST-elevation myocardial infarction (NSTEMI).
SUBJECTS AND METHODS
A total of 131 NSTEMI patients with moderate-high Thrombolysis in Myocardial Infarction risk scores, who had been admitted to our department between July 2011-December 2011 were included in our study. They had been randomized into 2 groups according to the timing of the percutaneous coronary intervention (PCI). Patient undergoing PCI in the first 24 hours of hospitalization were named the "Early Invasive Group" and those undergoing PCI between 24-72 hours of hospitalization were named the "Delayed Invasive Group". All patients were followed up for 3 months.
RESULTS
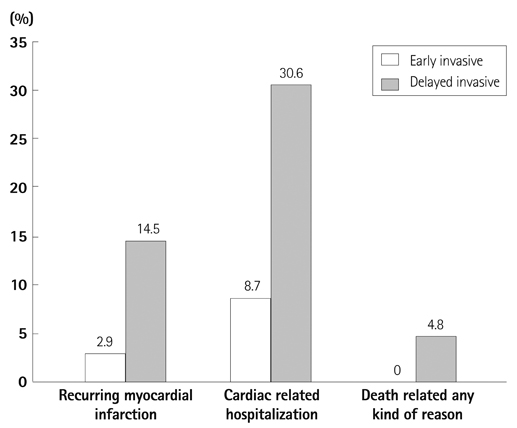
Third month left ventricular ejection fraction (LVEF) values were higher in the early invasive group (59.9+/-6.0% vs. 54.1+/-8.7%; p<0.001). Recurrent MI rates were lower in the early invasive group (2.9% vs. 14.5%; p=0.016). Similarly, hospitalization rates due to cardiac events were lower in the early invasive group (8.7% vs. 30.6%; p=0.001). All cause mortality appeared to be lower in the early invasive group, although not to a statistically significant degree (0% vs. 4.8%; p=0.065).
CONCLUSION
The early invasive strategy appears to be more effective for the reduction of recurrent MI, re-hospitalization due to cardiac events, and the preservation of 3rd month LVEF in patients with moderate-high risk NSTEMI when compared to a delayed invasive strategy.
MeSH Terms
Figure
Cited by 1 articles
-
Therapeutic Hypothermia for Cardioprotection in Acute Myocardial Infarction
In Sook Kang, Ikeno Fumiaki, Wook Bum Pyun
Yonsei Med J. 2016;57(2):291-297. doi: 10.3349/ymj.2016.57.2.291.
Reference
-
1. Mehta SR, Cannon CP, Fox KA, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: a collaborative meta-analysis of randomized trials. JAMA. 2005; 293:2908–2917.2. Patel TN, Bavry AA, Kumbhani DJ, Ellis SG. A meta-analysis of randomized trials of rescue percutaneous coronary intervention after failed fibrinolysis. Am J Cardiol. 2006; 97:1685–1690.3. Katritsis DG, Siontis GC, Kastrati A, et al. Optimal timing of coronary angiography and potential intervention in non-ST-elevation acute coronary syndromes. Eur Heart J. 2011; 32:32–40.4. Bigi R, Cortigiani L, Colombo P, Desideri A, Bax JJ, Parodi O. Prognostic and clinical correlates of angiographically diffuse non-obstructive coronary lesions. Heart. 2003; 89:1009–1013.5. Savonitto S, Ardissino D, Granger CB, et al. Prognostic value of the admission electrocardiogram in acute coronary syndromes. JAMA. 1999; 281:707–713.6. Volmink JA, Newton JN, Hicks NR, Sleight P, Fowler GH, Neil HA. The Oxford Myocardial Infarction Incidence Study Group. Coronary event and case fatality rates in an English population: results of the Oxford myocardial infarction incidence study. Heart. 1998; 80:40–44.7. Terkelsen CJ, Lassen JF, Nørgaard BL, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005; 26:18–26.8. Hamm CW, Bassand JP, Agewall S, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2999–3054.9. Neumann FJ, Kastrati A, Pogatsa-Murray G, et al. Evaluation of prolonged antithrombotic pretreatment ("cooling-off" strategy) before intervention in patients with unstable coronary syndromes: a randomized controlled trial. JAMA. 2003; 290:1593–1599.10. Sorajja P, Gersh BJ, Cox DA, et al. Impact of delay to angioplasty in patients with acute coronary syndromes undergoing invasive management: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) trial. J Am Coll Cardiol. 2010; 55:1416–1424.11. de Winter RJ, Windhausen F, Cornel JH, et al. Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med. 2005; 353:1095–1104.12. Mehta SR, Granger CB, Boden WE, et al. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009; 360:2165–2175.13. Riezebos RK, Ronner E, Ter Bals E, et al. Immediate versus deferred coronary angioplasty in non-ST-segment elevation acute coronary syndromes. Heart. 2009; 95:807–812.14. Montalescot G, Cayla G, Collet JP, et al. Immediate vs delayed intervention for acute coronary syndromes: a randomized clinical trial. JAMA. 2009; 302:947–954.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Consecutive Multivessel Myocardial Infarction during Primary Percutaneous Coronary Intervention
- Missing Right Coronary Artery in a Patient with Acute Inferior ST Segment Elevation Myocardial Infarction: A Case of Extremely Rare Variation of Coronary Anatomy
- A Case of Coronary Artery Dissection after Blunt Chest Trauma Resulting in ST-Segment Elevation Myocardial Infarction
- The Operator Volume of Primary Percutaneous Coronary Intervention for ST Segment Elevation Myocardial Infarction Does Not Guarantee Its Quality in Korea