J Rheum Dis.
2012 Aug;19(4):212-215. 10.4078/jrd.2012.19.4.212.
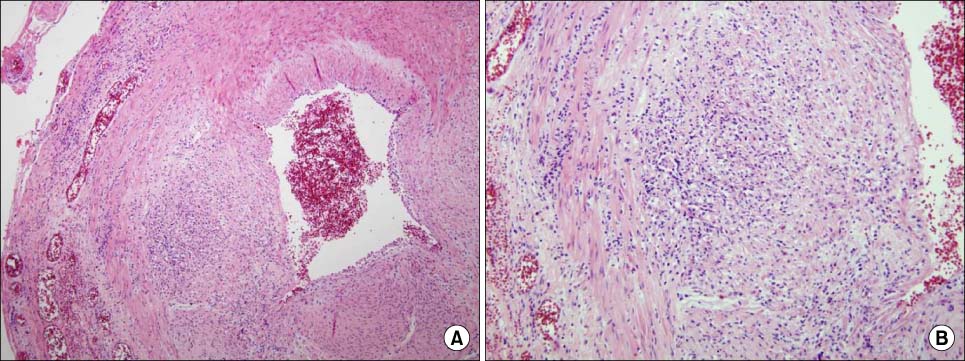
A Case of Giant Cell Arteritis Accompanied by Acute Myeloid Leukemia
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. shlee@kuh.ac.kr
- KMID: 2223073
- DOI: http://doi.org/10.4078/jrd.2012.19.4.212
Abstract
- Giant cell arteritis (GCA), the most common form of systemic vasculitis in adults, preferentially involves large and medium-sized arteries in patients over the age of 50. The classic manifestations are headaches, jaw claudication, polymyalgia rheumatica, and visual symptoms. Acute myeloid leukemia (AML) is a hematopoietic stem cell disorder characterized by a block in the differentiation of hematopoiesis, resulting in the growth of a clonal population of neoplastic cells or blasts. This malignant alteration in hematopoietic stem cells leads to a loss of normal hematopoietic function, which, if left untreated, typically leads to death within weeks to months of its clinical presentation. Although there have been reports of CLL or CML accompanied by several kinds of autoimmune vascular diseases, such as polymyalgia rheumatica, GCA, or necrotizing temporal arteritis, no studies have reported a case of AML with GCA. We experienced an 80-year-old male patient who developed AML 6 years after the diagnosis of GCA. He was under the use of oral glucocorticoid, hydroxychloroquine, and methotrexate at the time of the diagnosis of the AML. This is the first case in Korea to report GCA accompanied by AML.
MeSH Terms
Figure
Reference
-
1. Levine SM, Hellmann DB. Giant cell arteritis. Curr Opin Rheumatol. 2002. 14:3–10.2. Fain O, Hamidou M, Cacoub P, Godeau B, Wechsler B, Pariès J, et al. Vasculitides associated with malignancies: analysis of sixty patients. Arthritis Rheum. 2007. 57:1473–1480.3. Hamidou MA, Boumalassa A, Larroche C, El Kouri D, Blétry O, Grolleau JY. Systemic medium-sized vessel vasculitis associated with chronic myelomonocytic leukemia. Semin Arthritis Rheum. 2001. 31:119–126.4. Anderson LA, Pfeiffer RM, Landgren O, Gadalla S, Berndt SI, Engels EA. Risks of myeloid malignancies in patients with autoimmune conditions. Br J Cancer. 2009. 100:822–828.5. Shipley JL, Butera JN. Acute myelogenous leukemia. Exp Hematol. 2009. 37:649–658.6. González-Gay MA, Blanco R, González-López MA. Simultaneous presentation of giant cell arteritis and chronic lymphocytic leukemia. J Rheumatol. 1997. 24:407–408.7. Warrington KJ, Scheithauer BW, Michet CJ. Acute myeloid leukemia associated with necrotizing temporal arteritis. J Rheumatol. 2003. 30:846–848.8. von Knorring J, Somer T. Malignancy in association with polymyalgia rheumatica and temporal arteritis. Scand J Rheumatol. 1974. 3:129–135.9. Wang X, Hu ZP, Lu W, Tang XQ, Yang HP, Zeng LW, et al. Giant cell arteritis. Rheumatol Int. 2008. 29:1–7.10. Park MJ, Choi HB, Yoon HY, Choi EJ, Kim SY, Kim HJ, et al. Susceptibility of leukemia according to the genotype of minor histocompatibility antigens in a Korean population. Korean J Hematol. 2007. 42:15–23.11. Kim HD, Hwang JS, Cho YJ, Han NM, Jung KY. A case of adult acute myeloid leukemia presenting with musculoskeletal manifestations. J Korean Rheum Assoc. 2009. 16:144–149.12. Haga HJ, Eide GE, Brun J, Johansen A, Langmark F. Cancer in association with polymyalgia rheumatica and temporal arteritis. J Rheumatol. 1993. 20:1335–1339.13. Liozon E, Loustaud V, Fauchais AL, Soria P, Ly K, Ouattara B, et al. Concurrent temporal (giant cell) arteritis and malignancy: report of 20 patients with review of the literature. J Rheumatol. 2006. 33:1606–1614.14. Ji J, Liu X, Sundquist K, Sundquist J, Hemminki K. Cancer risk in patients hospitalized with polymyalgia rheumatica and giant cell arteritis: a follow-up study in Sweden. Rheumatology (Oxford). 2010. 49:1158–1163.15. Myklebust G, Wilsgaard T, Jacobsen BK, Gran JT. No increased frequency of malignant neoplasms in polymyalgia rheumatica and temporal arteritis. A prospective longitudinal study of 398 cases and matched population controls. J Rheumatol. 2002. 29:2143–2147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Giant cell arteritis of the breast: a case report
- A Case of Giant Cell Arteritis developed in Polymyalgia Rheumatica
- Acute Myeloid Leukemia with Intracardiac Thrombus Presenting as Acute Limb Ischemia
- A Case of Cerebral Infarction Associated with Giant Cell Arteritis
- A Case of Myeloid Sarcoma Preceding the Diagnosis of Acute Myeloid Leukemia